Developing the academic radiographer of the future
There is a growing demand for academic radiography practitioners to provide quality education with modern relevance

The evolving role of the radiographer has directly influenced the provision of contemporary patient care pathways. Evidence-based clinical radiography practice is increasingly being promoted as education and research has become an integral pillar of the profession1.
The changing clinical landscape requires radiographers with knowledge and competence to adapt to quickly evolving situations, including engagement in continuous professional development and learning to perform efficiently in advanced practice roles2. For example, most extended clinical scope of practice skills seen in the last century – including vetting and treatment verification, cannulation and image evaluation – are now an expectation of threshold radiography competencies at qualification.
The current practitioner-level knowledge, skills and attributes include critical appreciation of the roles “disruptive technologies” play in the delivery of healthcare services1,3. Thus, the development of the radiographer of the future, with the relevant competence to address current clinical challenges, requires academic radiography practitioners with enhanced skillsets and knowledge to provide quality education of modern relevance2.
Over the past two decades, there has been a move to ensure the space between theory and practice is closely entwined, with many radiography programmes of study undertaking problem-based and enquiry-based learning as useful pedagogical models of scaffolding learning, teaching and assessments for the creation and attainment of the graduate-level outcomes4. Within the context of the higher education environment, this has been a potential route of career development for radiographers and both authors of this paper are examples of where this has been the case (See Table 1).
Table 1
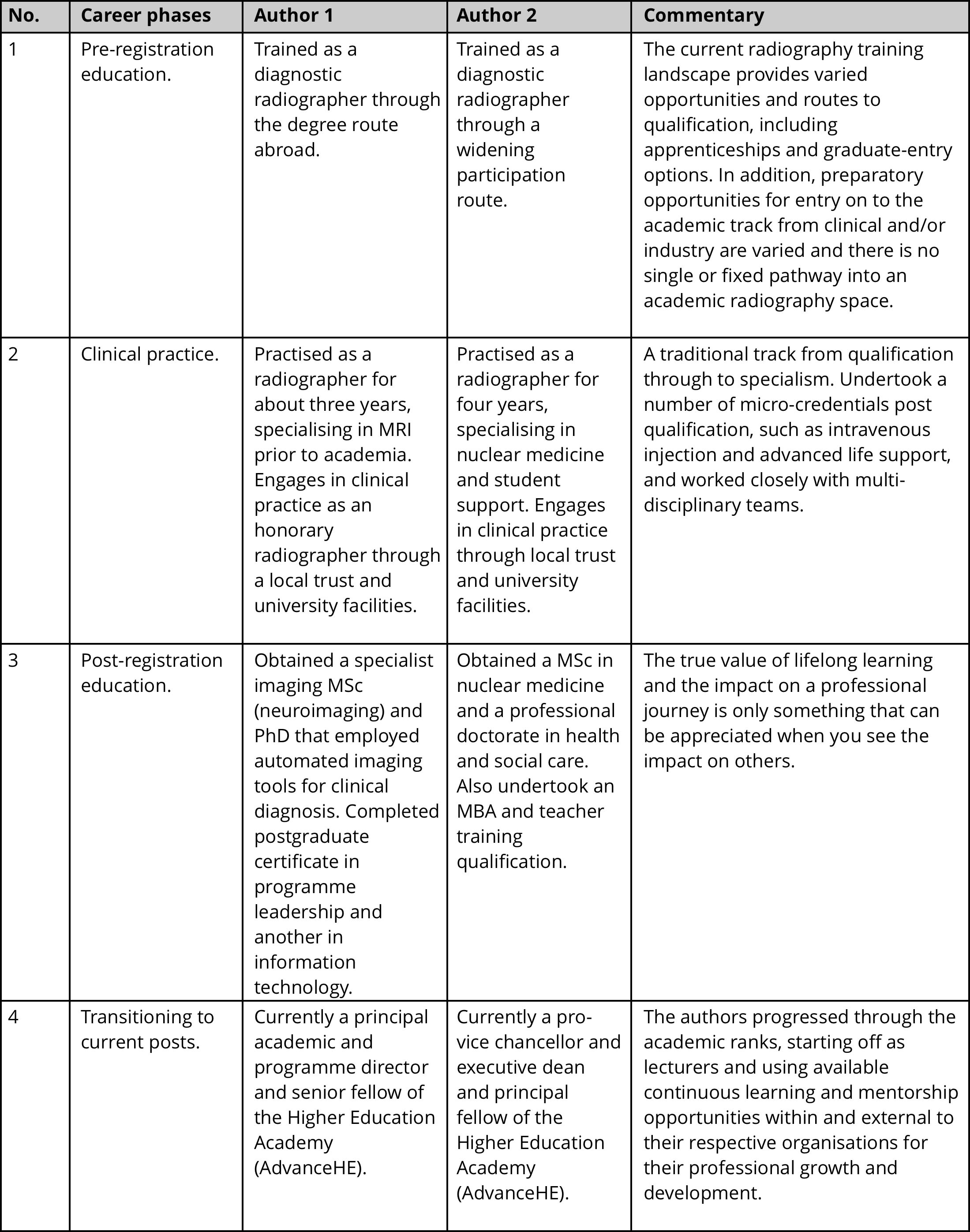
Table 1. Reflective commentary of the authors’ career trajectories into the contemporary academic space following radiography qualification
Over the past 10 years, the synergies between practice and higher education environments have seen advancements in leadership, research, service improvement and the provision of professional development at pre-registration and at post-registration. In addition, the development of third-space5,6 working environments within academia offers hybrid opportunities, particularly for professional groups, such as radiographers and other allied health professions (AHPs). A catalyst for such opportunities has undoubtedly arisen from the Covid-19 pandemics’ impact across the sector7,8, which has created greater permeability and agility for leadership and new ways of working9. Many radiographers who work within academia now find themselves acting as leaders of change, coaching and mentoring and supporting colleagues to develop their skills8, 10-12.
The findings of the Gravity Assist report by Sir Michael Barber13 have created the momentum, through the experiences of the Covid-19 pandemic and wider societal changes, to highlight the potential to shape a new wave of academic radiographers. This evolution resonates with the wider purpose of modern universities, which is to focus on social responsibility, learning and research14,15.
Our high-level article highlights exemplar career trajectories to an academic radiography career and provides insights into the emerging knowledge, skills and values that are being sought within academic spaces to support students and future learning, teaching and research endeavours.
Transitioning into a contemporary academic space

The movement into an academic role has undergone a transition over the past decade and there are now a number of models that support the career pathway of a radiographer who would like to move into a university environment (see Figure 1).
Figure 1
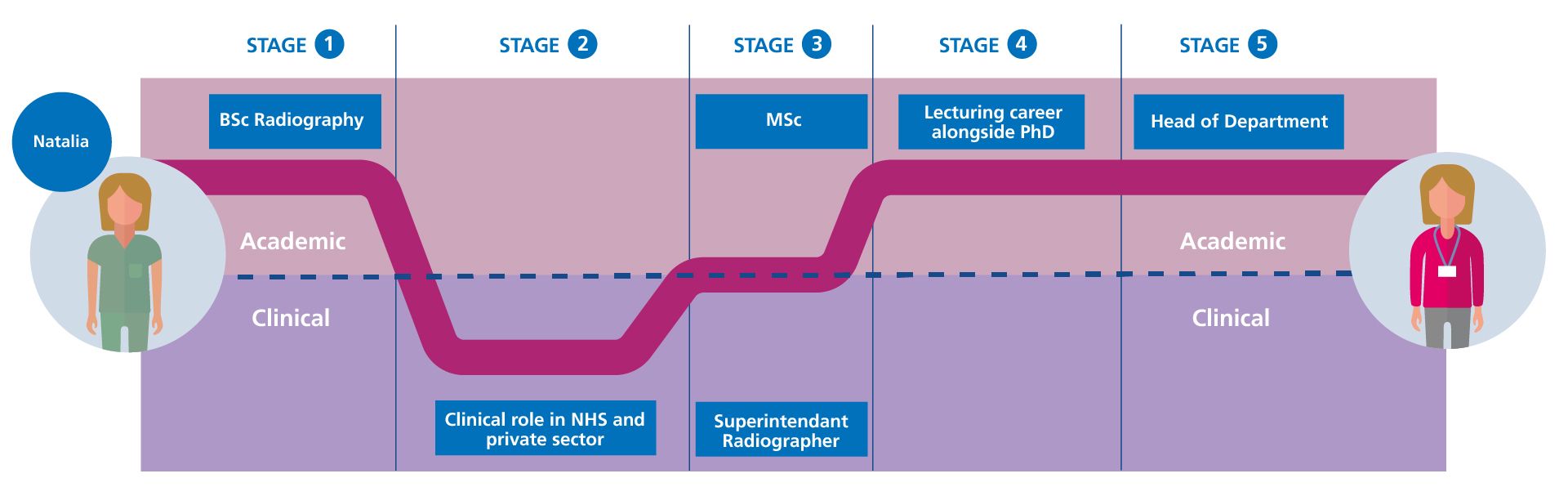
Figure 1a.
Stage 1 – Natalia completed a BSc radiography degree.
Stage 2 – Worked for 12 years in a clinical role in the NHS and the private sector.
Stage 3 – Became a superintendent radiographer for 4 years – alongside this, undertook an MSc.
Stage 4 – Decided to move into education and worked for 8 years as a lecturer while completing a PhD.
Stage 5 – Took on an externally funded project, gaining additional skills, before being offered a role as head of department.
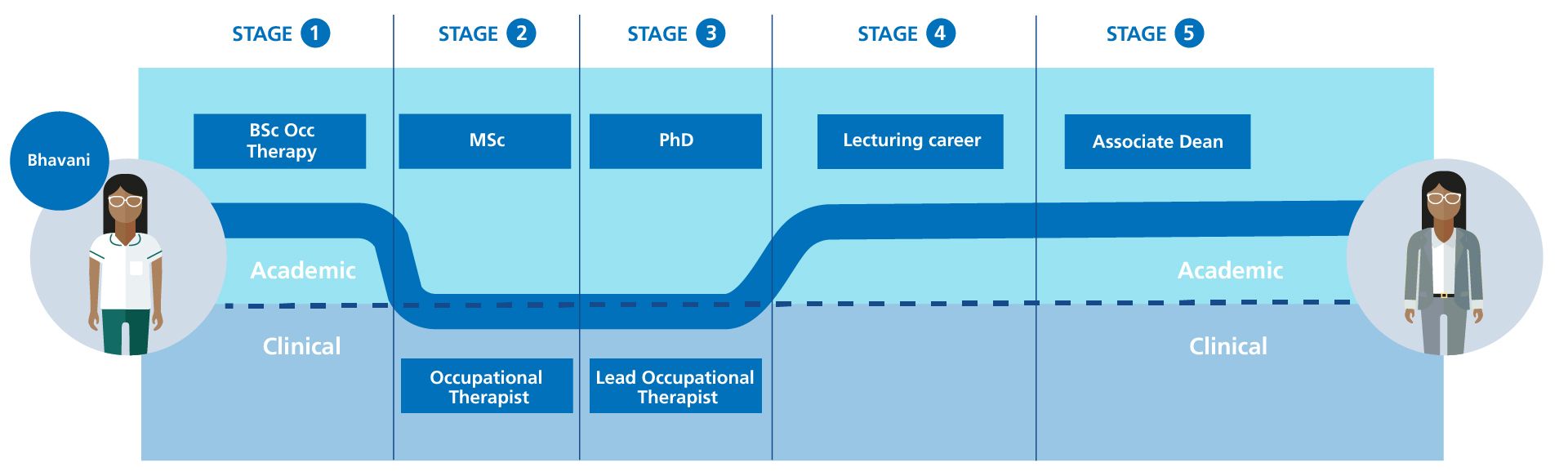
Figure 1b.
Stage 1 – Bhavani completed a BSc in occupational therapy.
Stage 2 – Worked clinically for 10 years in the NHS, developing a clinical specialism. Alongside this, she continued to study – first to MSc level and then to PhD level.
Stage 3 – While studying for her PhD, she was made lead occupational therapist.
Stage 4 – Commenced a lecturing career within a higher education institute.
Stage 5 – Took on additional responsibilities within the faculty, eventually gaining a role as associate dean.
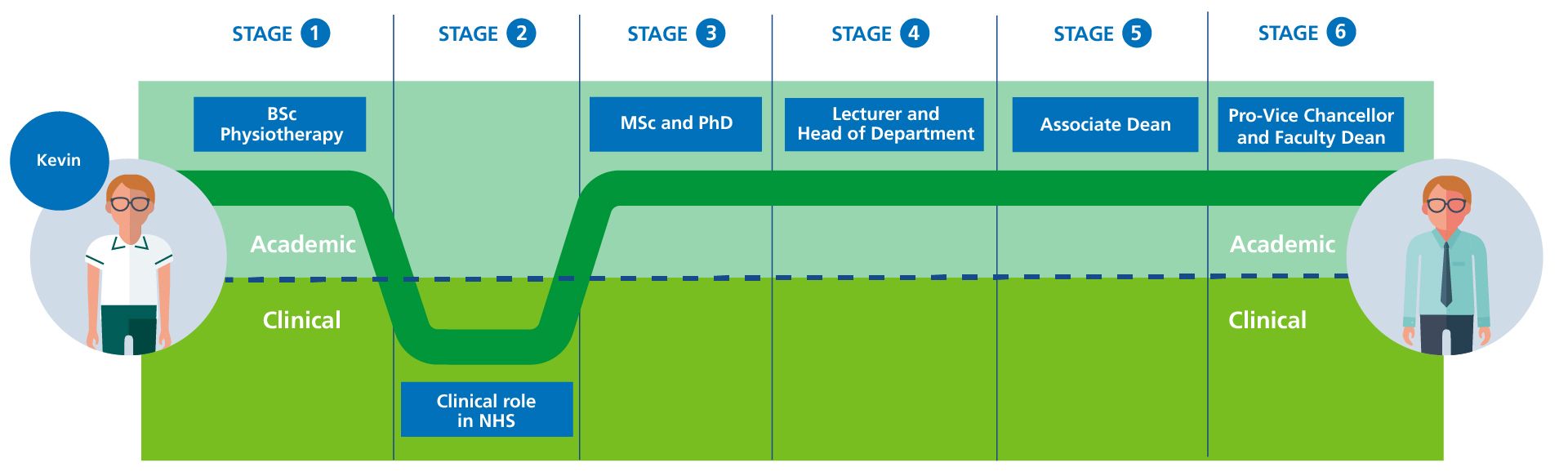
Figure 1c.
Stage 1 – Kevin completed a BSc physiotherapy degree.
Stage 2 – Worked for 2 years clinically in the NHS.
Stage 3 – Decided to move into academia to gain an MSc and a PhD.
Stage 4 – Worked for 6 years as a lecturer and took on a role as head of department for 4 years.
Stage 5 – Became an associate dean.
Stage 6 – Became pro-vice chancellor and faculty dean.
Figure 1. Exemplar transitioning AHP routes into the contemporary academic space. Adapted from Gibbs V, Palombi A and Akudjedu T (2023)11
There is now a greater balance required of those who work in an academic environment in terms of the wider skillset required to support students. Examples include a greater focus on pastoral care and resilience, greater connection and adherence to various quality frameworks, such as the Teaching Excellence Framework and governance in the form of the Office for Students and, in some cases, the Office for Standards in Education, Children’s Services and Skills.
The role of an academic also involves acting as an advocate for positive change, supporting the wider endeavours of the profession as a whole and representation through research, quality improvement and ensuring the connections with clinical and community practice are as strong and effective as they can be. It is for this reason that many universities support clinical academic models in which there is a joint appointment and/or secondment of a staff member, whose time is split between the academic and clinical space5,16. There are also wider connections through to completing advanced practice qualifications and the provision of leadership support through programmes such as the Council of Deans of Health Student Leadership Programme.
Promoting a career within academia has required a degree of “de-mystification” and also promoting the connected benefits from adopting such a move from one defined space (that is, clinical and/or industry) to another. A series of integrated work pieces was undertaken around identifying opportunities, challenges and key leadership skills for AHPs10-12 and these identified the need for the following core attributes of those working within a contemporary academic space with provision for healthcare programmes, including radiography (Figure 2).
Figure 2
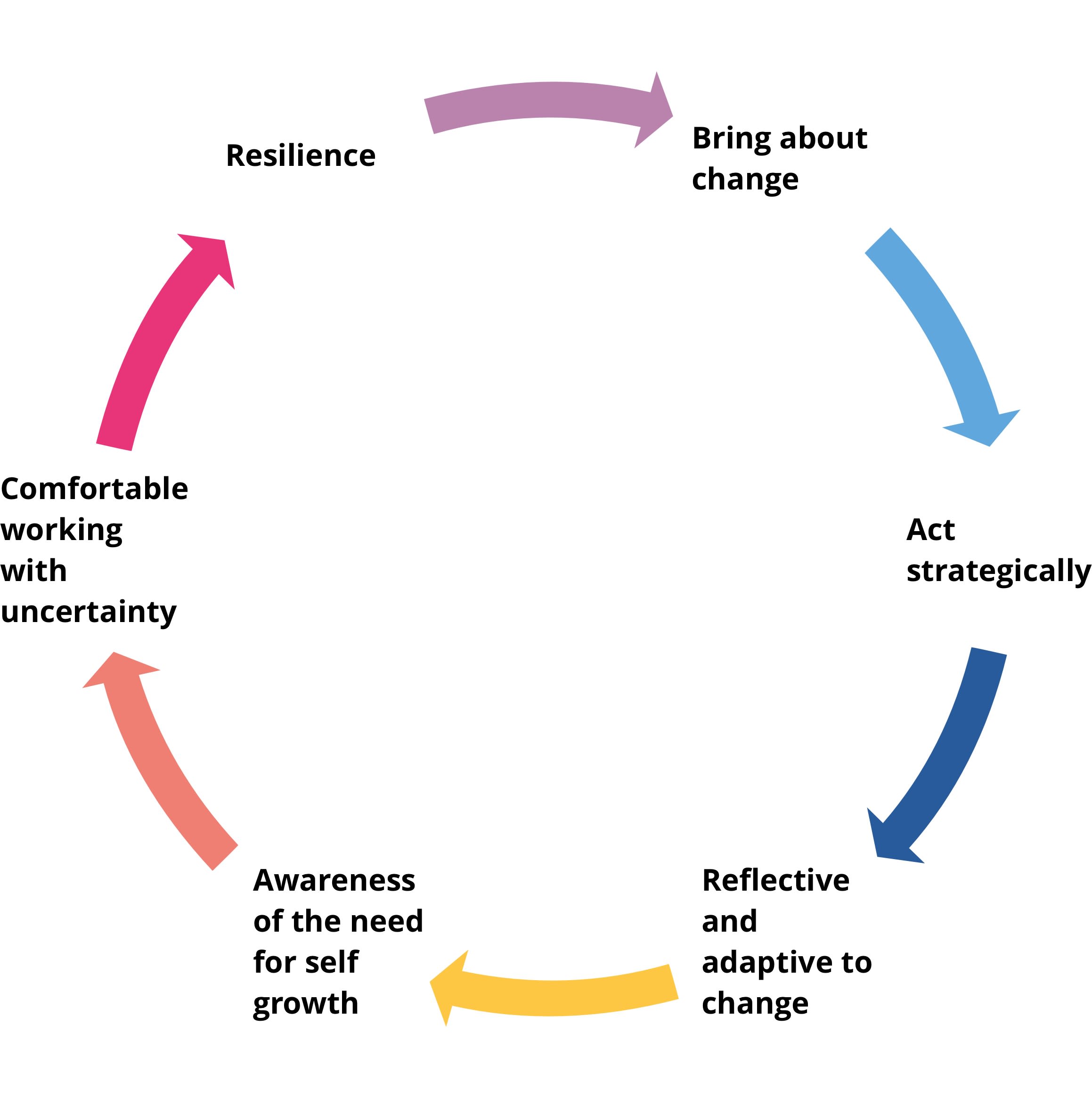
Figure 2. Core attributes for efficiency in the future academic space
Within the quickly evolving landscape of academic practice, additional competencies are required for effective operation in current and future radiography academic roles. For instance, the introduction of artificial intelligence (AI) and other new “disruptive” technologies in clinical radiography practice17 mean that both the academic and the clinical radiographer of the future need to learn new things, adapt and share knowledge differently.
Thus, these new competencies – including digital/simulated learning and professional growth – in the domain of management and leadership need to be weaved into the opportunities that being in academia present. As a profession, we need to continue to evolve and connect with other subject disciplines (AI/philosophy, creative industries, computer science and informatics, etc.) to develop a critical-thinking radiographer of the future.
The movement into an academic role has undergone a transition over the past decade and there are now a number of models that support the career pathway of a radiographer who would like to move into a university environment (see Figure 1).
Figure 1
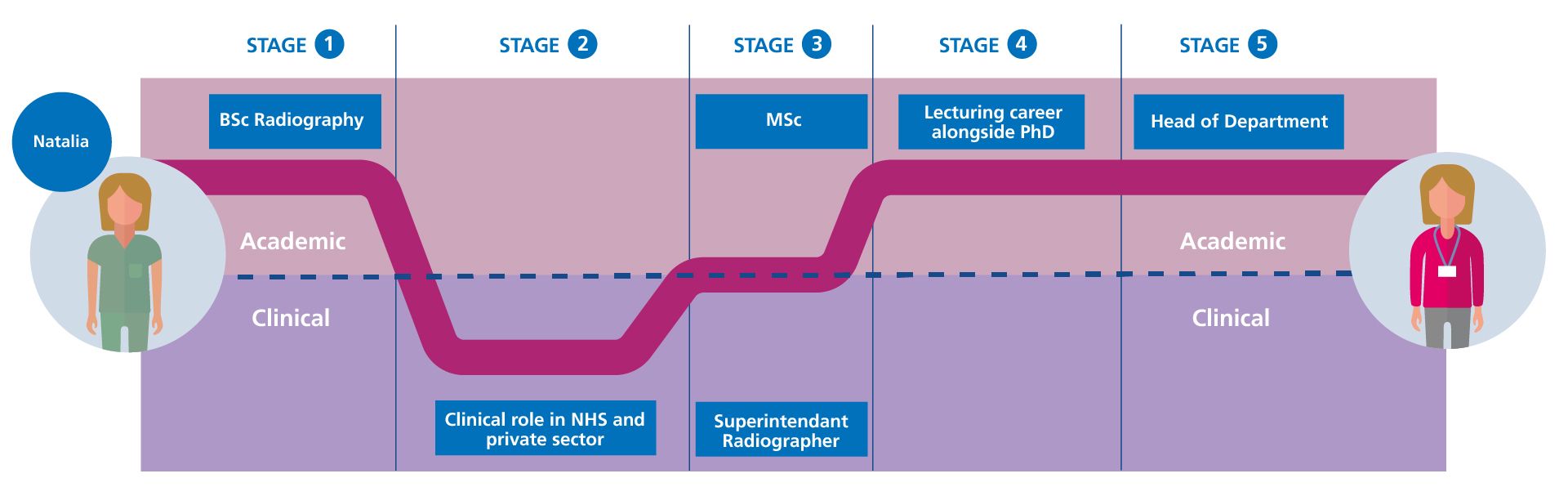
Figure 1a.
Stage 1 – Natalia completed a BSc radiography degree.
Stage 2 – Worked for 12 years in a clinical role in the NHS and the private sector.
Stage 3 – Became a superintendent radiographer for 4 years – alongside this, undertook an MSc.
Stage 4 – Decided to move into education and worked for 8 years as a lecturer while completing a PhD.
Stage 5 – Took on an externally funded project, gaining additional skills, before being offered a role as head of department.
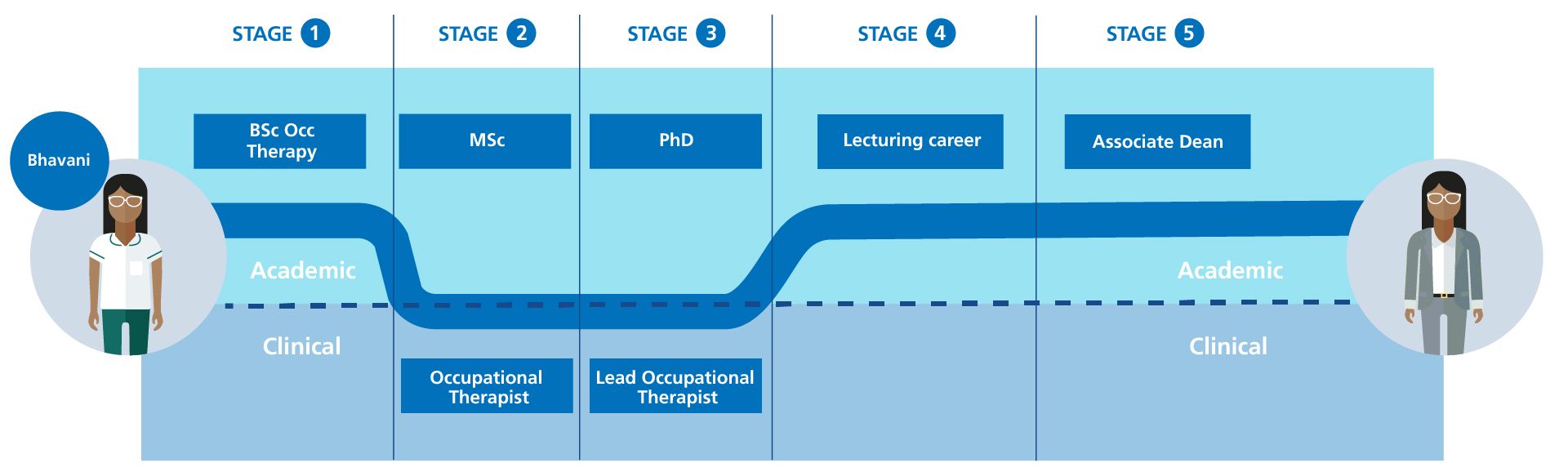
Figure 1b.
Stage 1 – Bhavani completed a BSc in occupational therapy.
Stage 2 – Worked clinically for 10 years in the NHS, developing a clinical specialism. Alongside this, she continued to study – first to MSc level and then to PhD level.
Stage 3 – While studying for her PhD, she was made lead occupational therapist.
Stage 4 – Commenced a lecturing career within a higher education institute.
Stage 5 – Took on additional responsibilities within the faculty, eventually gaining a role as associate dean.
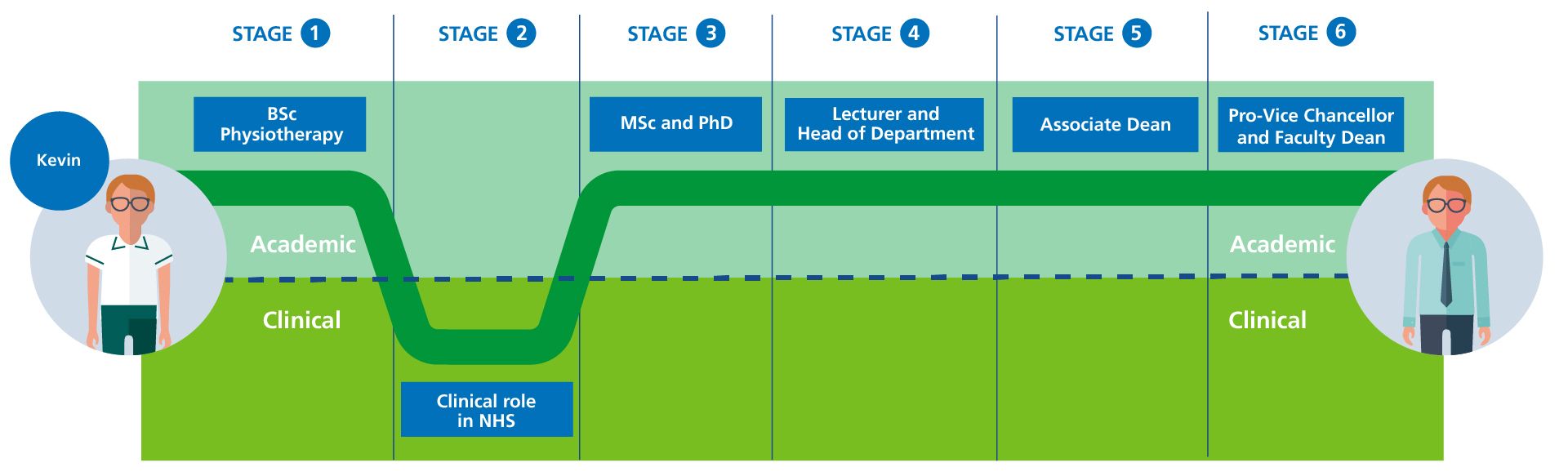
Figure 1c.
Stage 1 – Kevin completed a BSc physiotherapy degree.
Stage 2 – Worked for 2 years clinically in the NHS.
Stage 3 – Decided to move into academia to gain an MSc and a PhD.
Stage 4 – Worked for 6 years as a lecturer and took on a role as head of department for 4 years.
Stage 5 – Became an associate dean.
Stage 6 – Became pro-vice chancellor and faculty dean.
Figure 1. Exemplar transitioning AHP routes into the contemporary academic space. Adapted from Gibbs V, Palombi A and Akudjedu T (2023)11
There is now a greater balance required of those who work in an academic environment in terms of the wider skillset required to support students. Examples include a greater focus on pastoral care and resilience, greater connection and adherence to various quality frameworks, such as the Teaching Excellence Framework and governance in the form of the Office for Students and, in some cases, the Office for Standards in Education, Children’s Services and Skills.
The role of an academic also involves acting as an advocate for positive change, supporting the wider endeavours of the profession as a whole and representation through research, quality improvement and ensuring the connections with clinical and community practice are as strong and effective as they can be. It is for this reason that many universities support clinical academic models in which there is a joint appointment and/or secondment of a staff member, whose time is split between the academic and clinical space5,16. There are also wider connections through to completing advanced practice qualifications and the provision of leadership support through programmes such as the Council of Deans of Health Student Leadership Programme.
Promoting a career within academia has required a degree of “de-mystification” and also promoting the connected benefits from adopting such a move from one defined space (that is, clinical and/or industry) to another. A series of integrated work pieces was undertaken around identifying opportunities, challenges and key leadership skills for AHPs10-12 and these identified the need for the following core attributes of those working within a contemporary academic space with provision for healthcare programmes, including radiography (Figure 2).
Figure 2
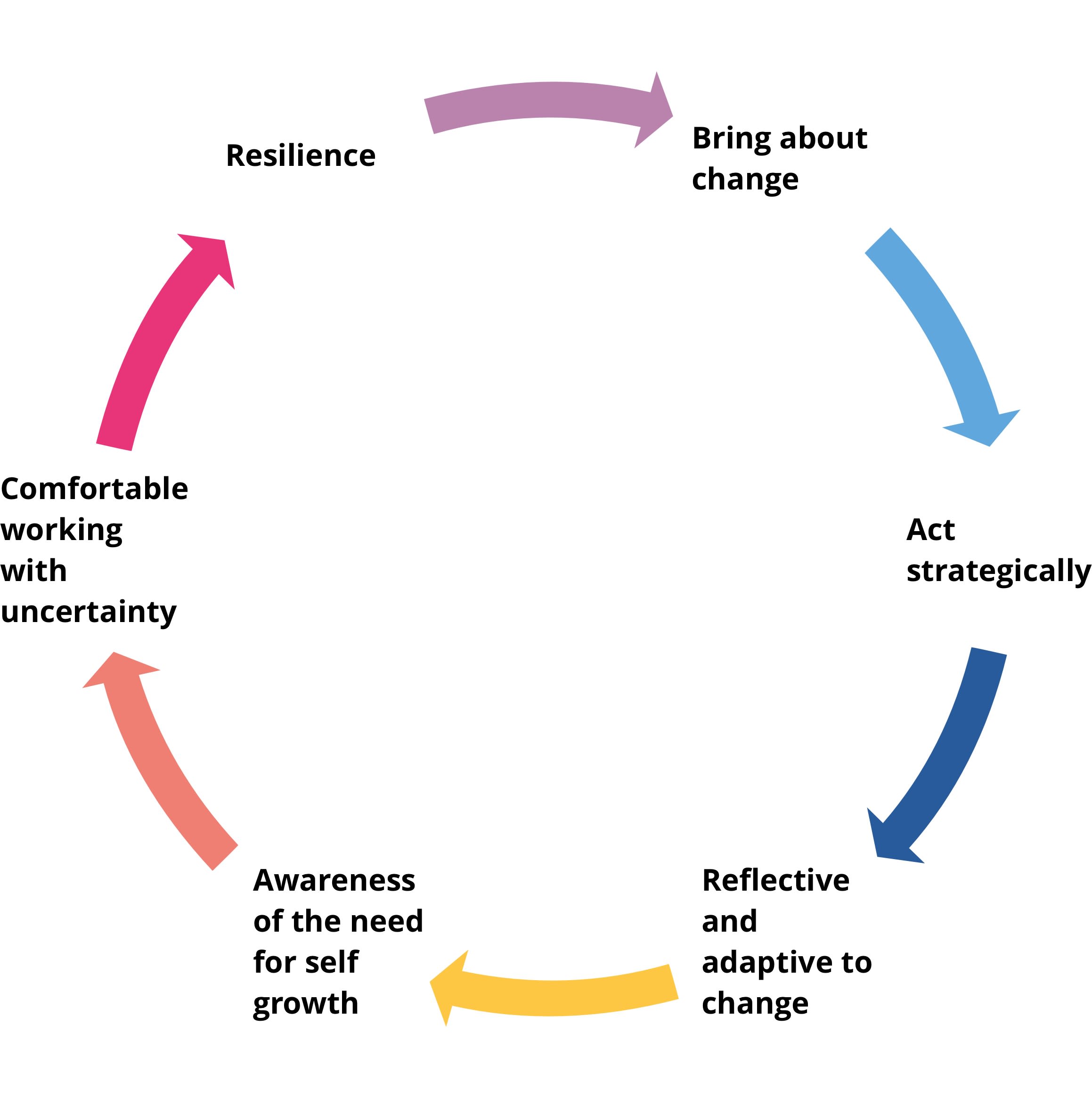
Figure 2. Core attributes for efficiency in the future academic space
Within the quickly evolving landscape of academic practice, additional competencies are required for effective operation in current and future radiography academic roles. For instance, the introduction of artificial intelligence (AI) and other new “disruptive” technologies in clinical radiography practice17 mean that both the academic and the clinical radiographer of the future need to learn new things, adapt and share knowledge differently.
Thus, these new competencies – including digital/simulated learning and professional growth – in the domain of management and leadership need to be weaved into the opportunities that being in academia present. As a profession, we need to continue to evolve and connect with other subject disciplines (AI/philosophy, creative industries, computer science and informatics, etc.) to develop a critical-thinking radiographer of the future.
Connecting with other subject disciplines

Radiography as a discipline integrates knowledge from other specialist fields, such as medicine, medical physics, nursing, computer science and information technology, among others. As part of students’ learning, it is therefore crucial to provide opportunities to connect with others from different disciplines both in practice-based and university environments. Hill et al.9 highlight the need for “creative abrasion, agility and resolution” within any space where there is opportunity for the creation of new knowledge and skills and, in this context, the outcomes include improved patient care.
These opportunities will prepare students to be innovative in readiness for the collaborative and multidisciplinary working approach that exist in all healthcare settings. Of note, the process of embedding interprofessional learning models remains a complex topic18. However, there exist opportunities for implementing this model for radiography education curriculums, especially in institutions where faculties are structured to oversee a range of healthcare and allied training programmes (see Figure 3).
Figure 3

Figure 3. A radiography academic and advanced practitioner in an enquiry-based learning session with students from a number of AHP subject disciplines
Digital and simulated learning

Working within the third space of academia5,6, there is a clear role for radiography academics to be leading the development and creation of simulated learning and practice. Established models of learning, such as problem and enquiry-based learning, have been proven as essential pedagogical approaches for the development of critical thinkers, who are able to adapt and make good clinical care decisions across varied settings while safely caring for patients4.
The outcomes of this scaffolding learning approach are powerful and relevant to the future needs, especially in a technologically dependent profession such as radiography. These outcomes require the radiography academic of the future to learn to understand and appreciate the integration of digital technology and its use for teaching and learning and in clinical practice.
The emergence of key publications over the past few years, such as commissioned work by Professor Eric Topol19 and Sir Michael Barber13, highlight the essence and key approaches to integrating these technologies for preparing the future healthcare professionals to deliver efficient care and in a safe manner.
In the pandemic, most radiography training institutions employed simulation activities to augment students’ learning and to make up for the clinical placement hours required for professional registration with statutory bodies. This phenomenon is expected to be normalised in the post-Covid era7,8.
Virtual reality learning was demonstrated to have a positive impact on the performance of students across a range of clinical radiography practice assessment domains, including patient positioning, exposure parameter selection and image appraisal. In a recent meta-synthesis20 that explored the clinical readiness of healthcare students (including radiography), the findings indicate that readiness was enhanced with increased use of simulation activities embedded into training programmes. These findings confirm the direction of teaching and learning of the future and, consequently, call on the radiography academic of the future to understand these technologies to be able to efficiently support student learning.
Barber13 highlights the need for several forces to come together to create an effective “gravity assist” and ensure the experiences of the Covid-19 pandemic are used to further enhance the educational offer for students. Radiographers and other AHPs are well positioned to further develop curricula, assessment designs and graduate outcomes with students and the pandemic innovation case studies from several universities4,5,8,14 highlight the work that has already been undertaken. Digital innovation, pedagogy redesign, technology enablement to create greater inclusive learning practices and change knowledge are all core competencies of the radiography profession and should also influence wider curricula design and strategic direction.
Applied data analytics and real-time feedback

The use of data analytics within the higher education sector has become crucial to business modelling and scenario planning. Having accurate and single point-of-truth data in areas such as student demographics, retention/engagement levels, learner engagement analytics and greater sector insight creates an opportunity to gather important data to either support existing curricula or research or accelerate a subject discipline.
Data is now so accessible in the modern learning environment, particularly with the advent of cloud-based and integrated learning platforms. Data tells us part of the narrative in relation to the engagement and wellbeing of students. However, it is the pastoral support provided by academics and the connection with wider university services, such as student support services, and wellbeing that has a significant impact on their progression and success.
Thus, the academic of the future needs to understand the wider interpretation and applied use of data to track student wellbeing for the provision of personalised pastoral care that enhances learning and the development of the softer skills that are so necessary within clinical practice.
The increase in awareness of mental health, and the various support pathways now in place across universities and clinical practice, also start to reshape the holistic and pastoral role of an academic and their understanding of learner engagement, data analytics and formative feedback loops from students.
Many universities are now starting to create stronger connections with local NHS services to ensure appropriate mental health support is available for students. Academics are also involved in training in the form of mental health first aid15. Furthermore, there is a need to ensure alternative ways of learning and engagement with the attitudes and behaviours of Gen Z students is firstly understood and embraced15.
Understanding student engagement and learning data is particularly crucial to consciously creating access and participation plans, which enhance inclusivity and improve student experiences. Radiographers are, by the very nature of their professional design, engaged in situations within the clinical environment that require team working, problem solving abilities and cognitive decision making.
Therefore, the professional makeup of modern radiographers who transition into academic spaces resonates with the emerging designs of universities in terms of shaping greater collaboration, leadership, professionalism and authentic followship, which dissolves traditional “frozen” cultures of organisations and begins to create third-space professionals5,6.
Research, industry partnerships and the evolving role of universities

The evolving role of universities and the nature of the work undertaken within society is changing. Practice-oriented programmes, which include radiography and other AHP subjects, have always connected with direct career links and strong employability opportunities, in contrast to subjects such as humanities.
Lifelong learning and continuing professional development have also long been key elements of the profession. However, this has now become a key aspect of modern academia and the interface of pastoral support and self and professional development are now expected across all subject disciplines, through graduate outcomes and other key metrics14.
It is for these reasons that radiographers are synchronised with the requirements of modern academia. The emergence of areas such as AI, simulation and integrated care pathways, for example, lend themselves to the core required skills and experiences of radiographers joining academia.
We should also remember that learning, research and innovation do not only take place in isolation within academia – the integration and links with clinical partners and wider third-sector organisations, including industry partnerships, is another example of where healthcare is already established in making a contribution to society. Radiography academics are now partnering industry to design, trial and provide user feedback through commissioned research initiatives for improved care.
In accordance with the College of Radiographers’ Education and Career Framework for the Radiography Workforce1, research is an important arm required for evidence-based practice so roles in research for radiographers across the NHS and universities are increasingly evolving. Similarly, academic radiographers are leading research activities as principal investigators across various methodological domains – as well as clinical conditions – with competitive funding awards from prestigious organisations.
Increasingly, academic radiographers are developing expertise in innovative methodological domains, such as citizen science and open-source learning/research (see Figure 4), and producing impactful research that improves wellbeing. These outcomes meet key metrics of the sectors’ research excellence framework.
Figure 4

Figure 4. A multi-professional approach to learning, involving a number of subject disciplines
In terms of postgraduate education to support research and personal development, there is a long-standing tradition of provision being undertaken through study at university, typically alongside an enhanced or advanced practitioner role and aligning with frameworks such as the College of Radiographers’ Education and Career Framework1.
Conclusion

The modern university requires an array of characteristics across key domains to support pastoral care, digital and simulated learning, research and enterprise, and understanding of data analytic tools for decision making in higher education. There is no single “pathway” into a career as an academic radiographer and/or an AHP educator. As highlighted by Gibbs and colleagues12, many AHPs move into the academic space after gaining some experience in clinical roles, while others focus on an academic pathway from early in their careers (see Table 1 and Figure 1).
The requirements of learners and future healthcare practitioners is evolving and broadening access to healthcare programmes, particularly for those who apply from underrepresented groups, needs to continue. This shift in some societal mindsets of what a university does and what it stands for needs to be advocated by those who learn and work in these organisations.
Timms and Heimans15 refer to the role and value of “New Power Universities” and their redress of purpose within society. Radiographers have the key knowledge, skills and ways of working to empower our future workforce but also ensure there is a professional disruption within wider professional groups.
Radiographers who want to move into the space where practice interfaces with curricula design, theoretical positioning and third-space working need to be encouraged through role modelling, active promotion and flexible approaches to employment contracts.
Dr Theophilus N Akudjedu is Principal Academic in Medical Imaging and MRI Radiography at Bournemouth University.
Professor Marc Griffiths is Pro-Vice Chancellor and Head of College for the College of Health, Science and Society at the University of the West of England.

References
1. The College of Radiographers. Education and Career Framework for the Radiography Workforce (fourth edition). 2022. Online, available at https://www.sor.org/getmedia/b2f6bf07-668f-4155-950a-b9d96c48eae1/12604-CoR-ECF-Interactive-v9a. Accessed 9 January 2023.
2. Snaith B and Beardmore C. Enhanced practice: a strategy to resolve the inconsistencies in advanced practice implementation. Radiography 2021. Volume 27, S3-S4.
3. Health and Care Professions Council. The Standards of Proficiency for Radiographers. 2023. Online, available at https://www.hcpc-uk.org/standards/standards-of-proficiency/radiographers/. Accessed 24 January 2023.
4. Lawal O, Ramlaul A and Murphy F. Problem-based learning in radiography education: a narrative review. Radiography 2020. Volume 27, Issue 2, 727-732.
5. McIntosh E, Nutt D. The Impact of the Integrated Practitioner in Higher Education: Studies in Third Space Professionalism. 2022. Oxon, Routledge.
6. Whitchurch C. The Rise of Third Space Professions: Paradoxes and Dilemmas. Cited in Teichler U and Cummings WC (Eds) Recruiting and Managing the Academic Profession. Dordrecht: Springer. Online, available at https://www.researchgate.net/publication/293098467_The_Rise_of_Third_Space_Professionals_Paradoxes_and_Dilemmas. Accessed 27 January 2023.
7. Akudjedu TN et al. The global impact of the Covid-19 pandemic on clinical radiography practice: A systematic literature review and recommendations for future services planning. Radiography 2021. Volume 27, Issue 4, 1219-1226.
8. Ofori-Manteaw BB et al. Impact of the Covid-19 pandemic on clinical radiography education: Perspective of students and educators from a low resource setting. Journal of Medical Imaging and Radiation Sciences 2021. Volume 53, Issue 1, 51-57.
9. Hill LA, Brandeau G, Truelove E and Lineback K. Collective Genius: the Art and Practice of Leading Innovation. 2014. Harvard Business Review Press.
10. Griffiths M and Gibbs V. Allied Health Profession Leadership in Academia: Opportunities, Challenges and Current Positioning. Council of Deans of Health and Health Education England. 2019. Online, available at https://councilofdeans.org.uk/wp-content/uploads/2019/09/UWE-HEE-CoDH-AHP-Leadership-Report-online-copy.pdf. Accessed 1 January 2023.
11. Gibbs V, Palombi A and Lawrence H. AHP Leadership in Academia: Skills and Attributes. Health Education England. 2021. Online, available at https://www.hee.nhs.uk/sites/default/files/documents/AHP%20Leadership%20paper_Project2_Final%20Jun21_Accessibility_version.pdf. Accessed 1 January 2023.
12. Gibbs V, Palombi A, Akudjedu T. An Interactive Roadmap for AHPs Considering a Career in Academia. Health Education England. 2023.
13. Barber, M and the Office for Students. Gravity Assist: Propelling Higher Education Towards a Brighter Future. Digital Teaching and Learning Review. 2021. Online, available at https://www.officeforstudents.org.uk/publications/gravity-assist-propelling-higher-education-towards-a-brighter-future/. Accessed 27 January 2023.
14. Byrne E and Clarke C. The University Challenge: Changing Universities in a Changing World. 2020. London, Pearson Education.
15. Timms H and Heimans J. New Power: How it’s Changing the 21st Century – and Why You Need to Know. 2018. New York, MacMillan.
16. Baltruks D and Callaghan P. Nursing, Midwifery and Allied Health Clinical Academic Research Careers in the UK. Council of Deans of Health. 2018. Online, available at https://councilofdeans.org.uk/wp-content/uploads/2018/08/Nursing-midwifery-and-allied-health-clinical-academic-research-careers-in-the-UK.pdf. Accessed 24 January 2023.
17. Akudjedu TN et al. Knowledge, perceptions and expectations of artificial intelligence in radiography practice: a global radiography workforce survey. Journal of Medical Imaging and Radiation Sciences 2023. Volume 0, Issue 0.
18. O’Leary N, Salmon N and Clifford AM. ‘It benefits patient care’: the value of practice-based IPE in healthcare curriculums. BMC Med Educ 20, 2020. 424.
19. Topol, E. NHS Constitution. The Topol Review: Preparing the Healthcare Workforce to Deliver the Digital Future. 2019. Online, available at https://topol.hee.nhs.uk/. Accessed 27 January 23.
20. Hazell L, Lawrence H and Friedrich-Nel H. Simulation-based learning to facilitate clinical readiness in diagnostic radiography. A meta-synthesis. Radiography 2020. 26: e238-e245.
