Enhanced level practice in radiography: Busting the myths
What is enhanced practice?
Probably the most important point to start this discussion is that the enhanced level practice is nothing new in radiography and has been in existence under many guises over the years. Often seen as a ‘specialist radiographer’ role, this enhanced level of practice is now identified in a wide range of documents such as the Education and Career Framework, The College of Radiographers, 2022 (1) and the NHS Long-Term Workforce Plan (2023) (2). So, in essence, what exactly is the enhanced level of practice?
Figure 1
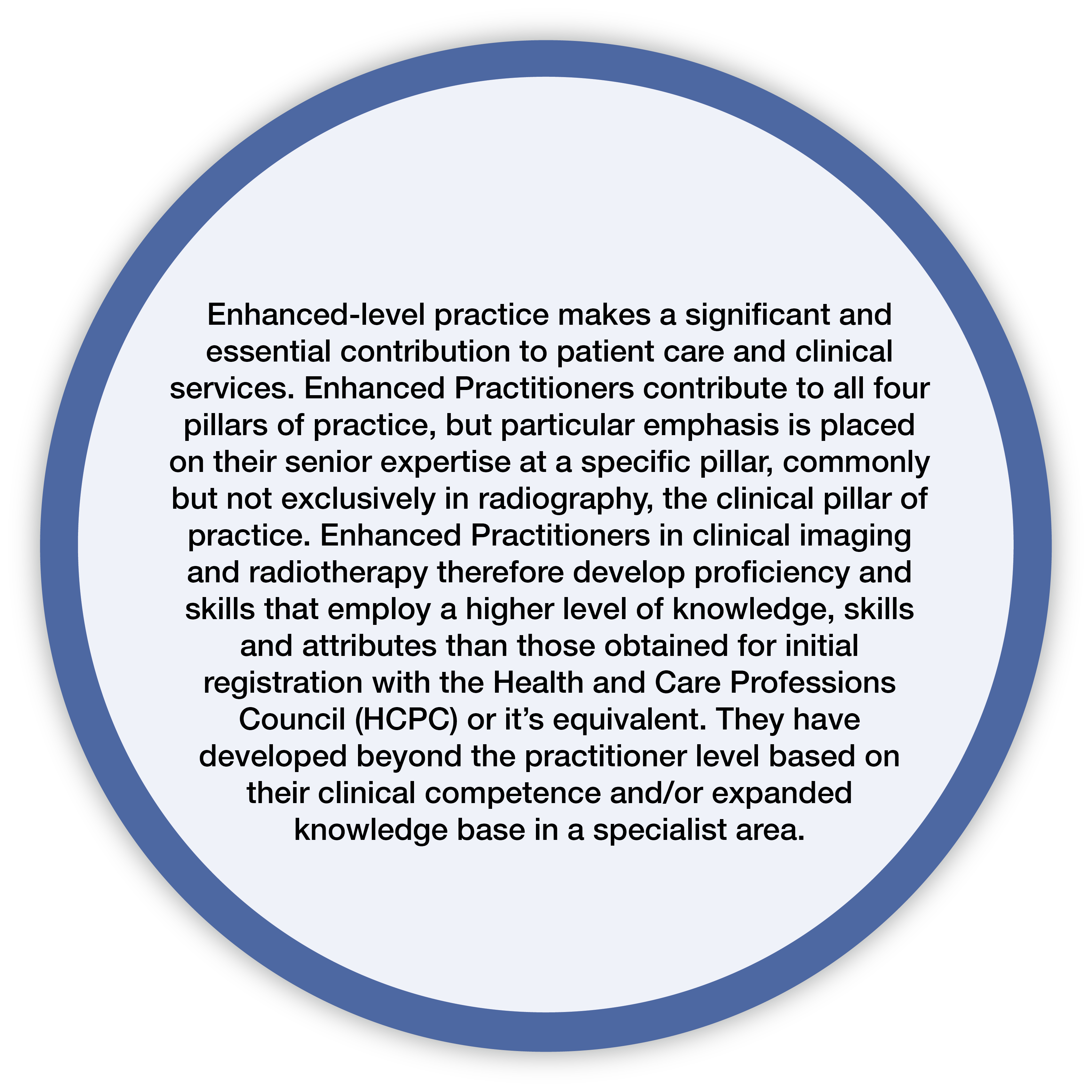
Figure 2
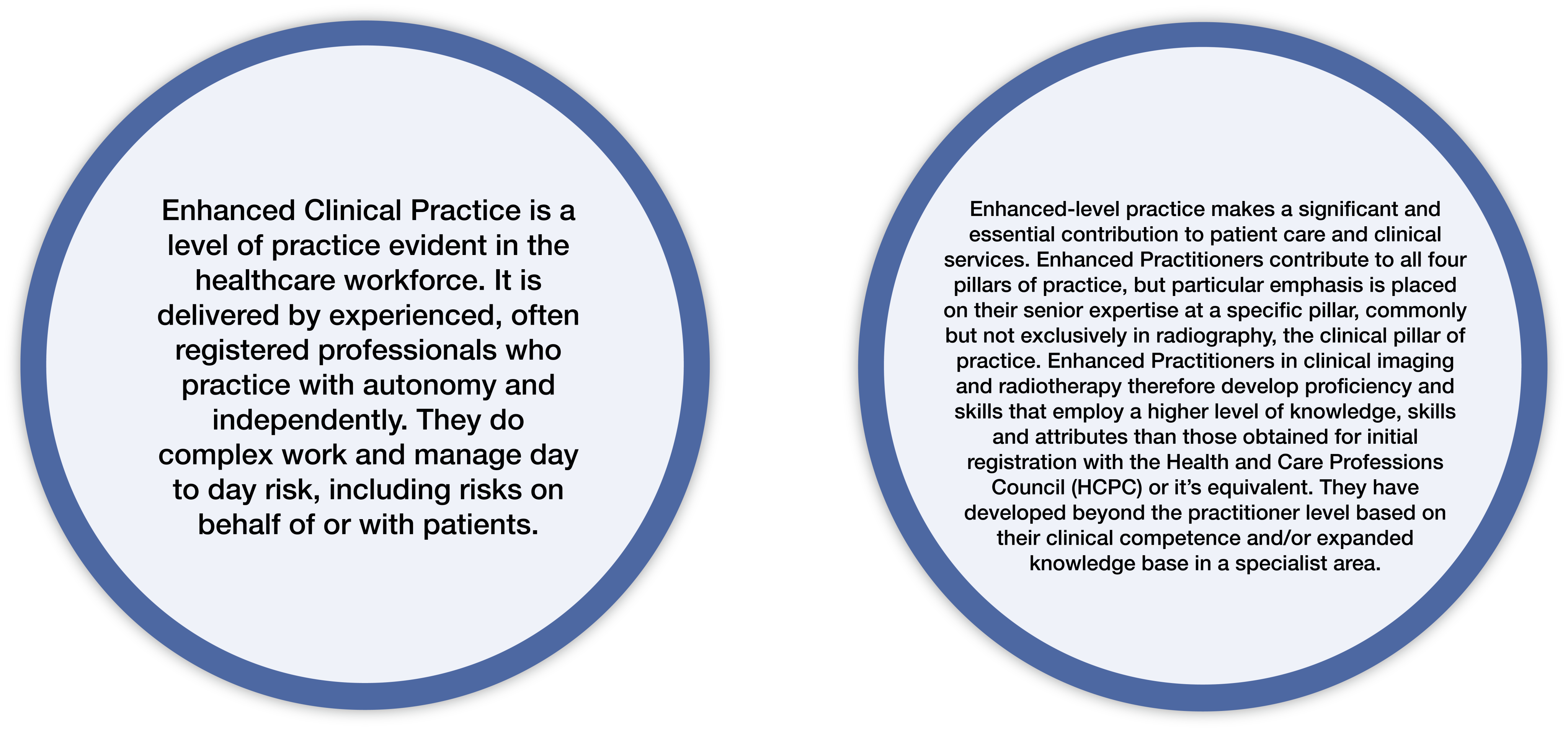
Figure 1
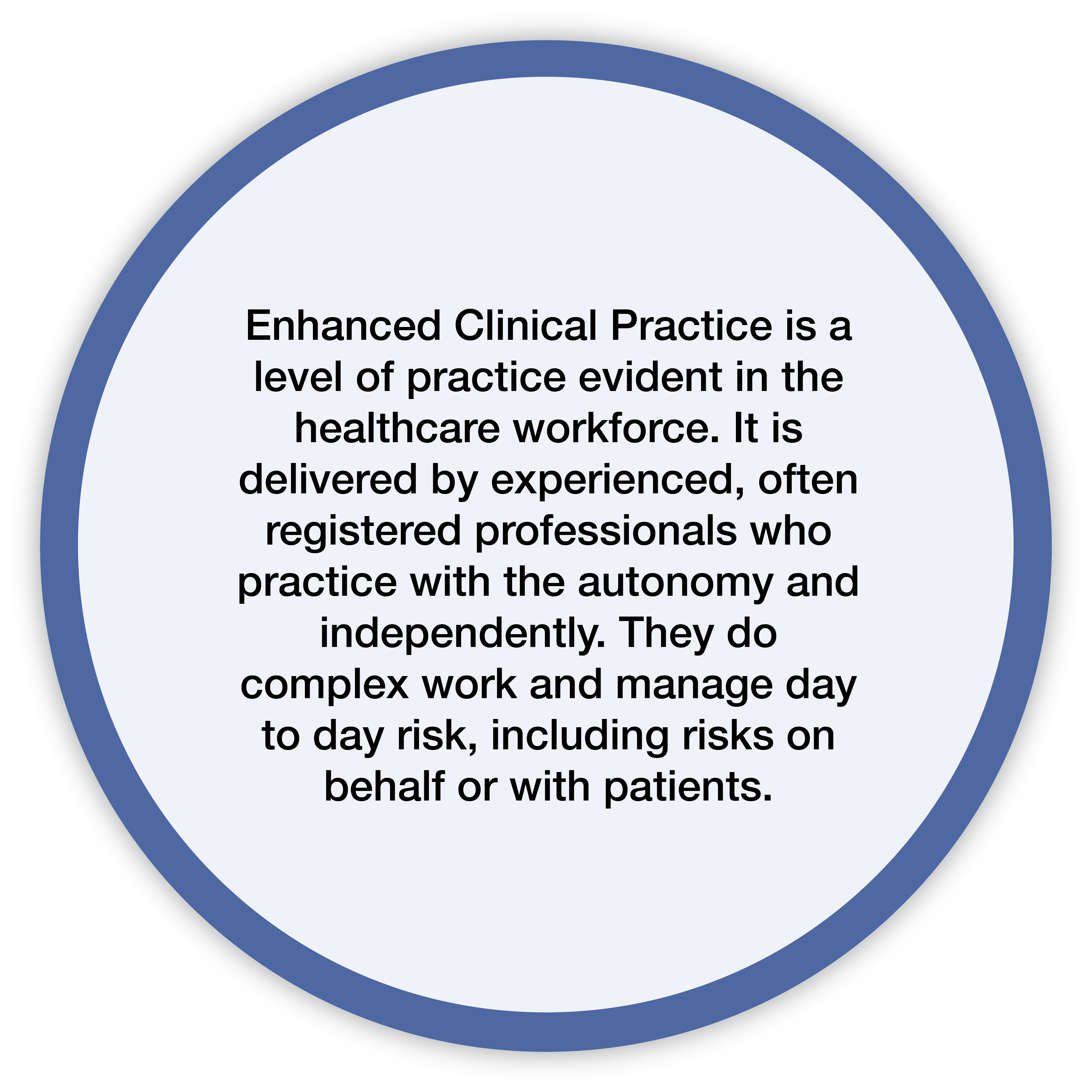
Figure 2
As with all levels of practice and identified within the ECF 2022 (1), the four pillars of practice are explicitly outlined and further defined. Figure 3 outlines the development and transitional relationship between the different levels of practice.
Figure 3
Figure 3
The enhanced level identifies autonomy in decision making alongside mitigating and managing risk within a defined scope of practice, which brings up the question of how this is different to the advanced level of practice. In all honesty, the answer lies in the scope of practice. It is this which clearly identifies the boundaries of the level of autonomy and the complexity of the clinical decisions that are being made. It is also important to acknowledge and consider that at an enhanced level, the practitioner could be operating significantly in any one of the pillars of practice.
The best way to describe enhanced level practice is to consider the terminology used by our nursing colleagues such as ‘door hanging’ (3). We all recognise this from our own practice where a practitioner has the experiential learning, knowledge, skills, and attributes to know the correct decision needing to be made in a situation, and yet they do not have the autonomy and responsibility to actually make that decision themselves. Ultimately, the decision ends up being made either by an advanced or consultant practitioner or by one of our medical colleagues. This scenario is common in many areas of practice and is deemed as lower risk in terms of its complexity.
It is acknowledged that identification of this level of practice has caused some uncertainty amongst the radiography community and this paper is aiming to demystify some of the more common myths and demonstrate the value of education and training that will provide a clear progression pathway within radiography.
Myth - What is an example of an enhanced clinical practitioner role?
It should be recognised that there is no dedicated enhanced clinical practitioner role. The confusion comes from the use of the apprenticeship model. In order to develop an apprenticeship standard, the requirement is that this must be aligned to a specific role. However, enhanced is the level of practice and is also not solely defined to the clinical pillar. There should be no introduction of new ‘enhanced practitioner’ titles and a clear reiteration to all, that the term ‘enhanced’ only represents the level of practice at which the individual operates at. It should also be noted that working at any level is not task orientated nor is it about task shifting. Another important point is that just because a certain task is completed by a certain practitioner, does not automatically indicate the level of practice they work at and so to conclude, it is the autonomy, responsibility and complexity of the decision making that defines the level of practice and not the task itself.
Myth - I am definitely an advanced practitioner and have been for a long time
With the recent review of titles on the NHS Electronic Staff Record (ESR), the Care Quality Commission (CQC) is interested in examining scopes of practice and training records of those using the word advanced within their title. This also reflects the recent moves within England to increase accreditation with the Centre for Advancing Practice (CfAP) which acts to recognise those working at an advanced level and the future potential for regulation of advanced practice. Job titles have and still are a hot topic for both organisations and professions, and it is acknowledged that within radiography, we have a significant misuse of the titles ‘advanced clinical practitioner’ and ‘advanced practitioner’, alongside a significant misunderstanding on how it applies to our specialty. It has been identified that many radiographers classifying themselves as an advanced practitioner are more likely to be aligned to and working at an enhanced level of practice. This is likely to be as a result of the hangover from the introduction of the four-tier structure (assistant practitioner, radiographer practitioner, advanced practitioner, and consultant practitioner) (5), where practitioners processed directly to advanced, with an absence of an interval step. The newfound emphasis on enhanced level practice will inevitably bring an increase in concern for many of these practitioners which is a completely understandable reaction. Often these individuals have worked very hard to get to the position they are in and there is also an element of professional identity and pride held within one’s title. Whilst this may bring feelings of unease amongst our professional community, it also brings the opportunity to embrace change, with an identified career pathway supported by a funded education and training route that is in alignment to our nursing and other Allied Health Profession (AHP) colleagues.
For those who feel they are effectively sandwiched between levels, the ECF 2022 (1) can support alongside the profession specific enhanced level practice schema that has recently been developed (4). This will aid practitioners to undertake a clearer learning needs analysis and identify gaps in their current education and training enabling them to plan a way to progress to the next level.
Myth - I will have to do additional education
New postgraduate courses will emerge over the next few years which are linked to the profession specific enhanced level schema (4). This will provide an opportunity for practitioners without academic qualifications to develop their skills and knowledge across all four pillars. As stated within the ECF 2022 (1), it is expected that practitioners working at this level of practice hold a postgraduate certificate as a minimum. Some practitioners who already hold postgraduate awards may want or need to broaden their skills to fill any identified gaps. Importantly the schema provides an expectation that practitioners will be able to accredit relevant prior learning towards their advanced practice master’s programme thereby enabling career progression if this is desired and needed by both the employer and the practitioner.
Myth - We can’t add this to the current workforce structure at this late stage
Developing across the four pillars of practice, the enhanced level will be played out through a variety of situations and roles that already exist in departments. This includes aspects such as team leadership in operational and clinical spaces, leading practice education provision across a clinical department which is inclusive of different levels of academia and working in research implementing clinical audits and trials. You will note that clinical examples have not been identified here because these as reiterated before, should be not task oriented. We urge practitioners to consider their local workplace and identify where they think enhanced level practice sits and how this could potentially feed into current and existing advanced and consultant level roles which serve to redefine services and support future succession planning.
Current work being undertaken in England in enhanced level practice

As previously alluded to, recent collaborative innovative partnerships, supported by NHS England, have undertaken the development of a schema and model curricular for enhanced level practice for both diagnostic and therapeutic radiography (4). These clearly define and outline the education and training required across the four pillars of practice at this level including the requirements in different specialities of radiography. The documents aim to guide Higher Education Institutes (HEIs) to develop post graduate education for practitioners who are aspiring to train and work at an enhanced level of practice. At present the favoured method of delivery may be through the designated apprenticeship however the schema and the model curricula are also relevant to all education routes at this level.
Wider considerations for Higher Education Institutes (HEI)

Many HEIs already provide education which is relevant to the enhanced level of practice, although similar to the current challenges in advanced practice these often will not include the breadth expected by the new frameworks being introduced. This again should be seen as an opportunity to develop the apprenticeship offering for the enhanced (and potentially advanced) level against the approved standards, designing specific programmes that provide exactly what service requires. It is not expected that this education provision will take over traditional postgraduate provision but should instead be seen as a way of maximising potential, promoting inclusivity, and facilitating an increase in employability offers for those completing programmes.
It is vital that HEIs start to include discussion at all levels of practice when introducing radiography career opportunities and future expectations for development across the different speciality areas. As well as providing a trajectory to consultant level practice, learners and practitioners should be encouraged to develop their careers through the Kawa growth-based career planning method (6).
“One way to structure growth-based career conversations is the Kawa approach. Kawa is Japanese for river. It invites us to think about our careers as individual rivers (not ladders), showing that they are part of the wider AHP ecosystem.” (7)
Managing expectations of current and future generational learners and practitioners is essential because the number of opportunities to progress to an advanced and consultant level is considerably less. This is clearly illustrated in figure 4 where we can see that the majority of the radiography workforce will operate at an enhanced level of practice for the duration of their career. Retention here will be key and so understanding and exploiting the broad depth of practice that the enhanced level will offer is essential.
Figure 4
Wider considerations for service managers

Ironically, it could be said that Radiography Service Managers (RSMs) are often overlooked when it comes to the dissemination of information on many accounts, and it appears where knowledge and awareness around the enhanced level of practice is concerned, this is no exception. When we consider the important and vital role that RSMs play within services, it seems obvious that they should be at the forefront of any type of discussion involving the development of the workforce. The intention of the discursive piece however is not to dwell on what isn’t happening or may have been lacking in the past but instead reiterate and highlight the importance that RSMs are both centrally placed and appropriately considered when it comes to the implementation of this ‘new’ level of practice.
RSMs are seen as being key to workforce transformation and planning within imaging and radiotherapy services and to undertake these activities efficiently and effectively, it is important they have a solid level of awareness and understanding around the different levels of practice. As reiterated previously, enhanced is not new and there has always been a level of practice situated between practitioner and advanced however, the more recent naming and clarification of this has led to confusion and uncertainty in multiple ways.
There are two specific areas where it is anticipated that RSMs will need to support and facilitate the successful implementation and utilisation of the enhanced level of practice. Firstly, is in those all-important career conversations that they hold with their staff members and secondly when they undertake and support workforce and succession planning activities that ultimately help shape and develop service delivery and patient care. It may be that conversations around implementation are already happening in the workplace, and if so then this should be seen as a positive step forward. If they aren’t, however, this then affords the RSM community a valuable opportunity to identify different types of resources that will ultimately support them in their knowledge and enable them to be proactive and on the front foot in their approach to the above.
There should be no underestimation of the important balancing role the RSM will need to play in the future when it comes to managing the expectations of keen staff who are eager to progress alongside the majority of the workforce who will use the enhanced level of practice as a career destination and not just as a stepping stone. Either way, it requires the RSM to take an informed and proactive standpoint so that aspects such as staff retention, service transformation and ultimately patient care and health outcomes, have the potential to benefit, improve and undergo further development.
Wider considerations for practitioners

We know that there is significant variation in roles, titles, pay level and opportunity across the UK and there is an expectation that the development of the enhanced level will result in greater harmonisation with clearer expectations on roles and responsibilities. For some, this may result in a change of role title, particularly if an individual is currently titled an ‘advanced practitioner’ but does not meet the expectations of this level. This should not, however, come with any change of pay band as it is acknowledged that this category will encompass a range of pay bands depending on the level of responsibility.
The opportunity for academic study with a clearer development pathway will be attractive for some and what should be celebrated is that importantly, enhanced level practice is inclusive of those in research, leadership, or education roles and is cognisant of that specific knowledge and skill set.
Enablers and barriers
Figure 5
|
Enablers |
Barriers |
|---|---|
|
Improve recruitment and retention |
Understanding and awareness of enhanced level practice |
|
A career destination |
Integration of enhanced level practice into strategic and local workforce planning |
|
Utilise the skill set of an experienced workforce |
The perceived uncertainty through a change in culture |
|
Have a positive impact on a change in culture. |
Lack of current education provision aligned to enhanced practice frameworks |
|
Effective and efficient workforce planning |
|
|
Clearer job descriptions |
|
|
Clear guidance on career progression |
|
|
Positive impact on patient care |
|
|
Education and training specific to practitioners' needs |
|
|
Reform service with innovative working practices |
In conclusion, it is acknowledged that this is a hot topic to discuss which may bring opposing views. Increasing and disseminating awareness alongside the strategic implementation of the enhanced level practice within services could bring both positivity and future development potential to the radiography profession. In this respect, we need to be both decisive and actionable in how we choose to embrace this.
References
- The College of Radiographers. (2022). The Education and Career Framework. Fourth Edition. London.
- NHS England. (2023). The NHS Long-Term Workforce Plan. London.
- Health Education England. (2022). The Principles of Enhanced Level Practice. London.
- NHS England (2024). Allied Health Professions Enhanced Level Practice Schemas with Model Curricula. London.
- Department of Health. (2003). Radiography Skills Mix: A report on the four-tier service delivery model. London.
- NHS England. (2024). Growth-based career planning. https://www.hee.nhs.uk/our-work/allied-health-professions/enable-workforce/growth-based-career-planning#:~:text='Kawa'%20is%20a%20Japanese%20term,career%20planning%20in%20recent%20years. Accessed 04/02/2024.
- NHS England (2024). Growing your AHP career. https://www.hee.nhs.uk/our-work/allied-health-professions/education-employment/national-allied-health-professionals-preceptorship-foundation-support-programme/growing-your#:~:text=One%20way%20to%20structure%20growth,of%20the%20wider%20AHP%20ecosystem. Accessed 04/02/2024.

