Q&A with Rachel Baldwin-Cleland
Breaking down the boundaries
Rachel Baldwin-Cleland, clinical research fellow at St Mark's Hospital in Harrow, London, tells Synergy why she became a radiographer, and how attitudes towards the profession have changed
Rachel Baldwin-Cleland
Rachel Baldwin-Cleland
Can you give us some background on your radiography experience?
I became a qualified diagnostic radiographer after completing my training at the University of Hertfordshire (UH) in 2003, and I started work at Northwick Park Hospital in North West London, the hospital where I did most of my placement training, and I am still employed by the trust today.
My initial passion was forensic radiography and I joined the Association of Forensic Radiographers very early on (I was an avid CSI: Vegas fan), but our trust didn’t have the facilities to set up a post mortem service, so I found a different career passion instead in gastrointestinal (GI) imaging.
I worked my way up, training in CT and fluoroscopy specifically and became the trust’s first research radiographer in 2010, covering every speciality, and then also took on the role of gastrointestinal superintendent radiographer at St Mark’s Hospital within the trust in 2011.
Northwick Park and St Mark’s Hospital in Harrow, North West London
Northwick Park and St Mark’s Hospital in Harrow, North West London
Management of a GI service came with its complexities and when I first started there were no supportive courses to help me with this so local mentorship was extremely helpful to me.
Along my career path I've undertaken a PgCert in CT in 2010, a facilitation in education in practice module in 2012, a MSc in Medical Imaging in Radiation Science in 2017, and a CT Colonography (CTC) reporting module in 2022.
I'm also very interested in clinical training and supervision since I started and was a radiography student coordinator link with UH for many years.
Since 2007, I've been actively involved in radiographer and radiologist CTC educational courses, at St Mark’s hospital and nationally.
The opportunity to develop a ‘train the trainers’ course specifically for radiographers has been an intensive but rewarding challenge, and we have also adapted and run them for radiologists, practice educators and now for the National CTC Training and Accreditation Programme (NCTCTAP).
As radiography professionals, we are expected to teach every day within our clinical setting, but we are never taught how to do that well in a one-to-one setting.
I was fortunate to co-chair and publish the National Best Practice Guidelines for Radiographer Training and Education in CTC (hosted on the SoR website here) in 2018 with Julie Nightingale and a great team from around the country.
I am co-author of two book chapters on CTC imaging within two editions now, and been involved in around 20 journal publications in GI imaging.
Since it's inception, I've sat on the Bowel Cancer Screening Radiology Quality Assurance Committee, helping to highlight the need for adequate training both for us and radiologists, and advocating for radiographers to also be leads within CTC services.
Rachel is a specialist in CT colonography
Rachel is a specialist in CT colonography
I don't have any qualms about reminding radiologists that radiographers are not their minions, though to be fair the tide of that opinion has definitely changed over the years I've been in the profession.
Our team have created, published and subsequently updated BCSP Imaging guidelines, which have been early implementers for other CTC guidance.
I am also lucky to be the chair of the Gastrointestinal Radiographers Special Interest Group (GIRSIG), which offers advice on GI imaging, and is in talks with the radiologist version of the group (the British Society of Gastrointestinal and Abdominal Radiology) about a merger. The professional boundaries are becoming less between the groups, so it makes sense to link up.
One of my top 10 achievements was being asked by SoR and the American Society of Radiologic Technologists to lecture for one hour at RSNA in Chicago on Radiographer CTC education and training within the UK in 2017. I caught the flu whilst there and don’t remember two of the days! I carried out my presentation loaded with so much medicine it was a complete blur, but on the bright side it really helped with the nerves!
In 2020 I was asked to join a secondment to help set up the National CTC Training and Accreditation Programme (NCTCTAP).
This, along with my previous career moves and networking, enabled me to be in a position to apply for a radiology registrar PhD post.
I persuaded the supervisors that I was uniquely positioned (and skilled) to fill the role as a radiographer, and they advertised the post without GMC registration as an essential.
I was intensely grilled at the interview but got the post, much to my relief! I had always wanted to take my research career further and a fully funded post is extremely rare for radiographers in a clinical setting.
So, I am one year into a seconded PhD studying at UCL whilst still working with NCTCTAP. It has been strange after 20-plus years not to go into a clinical setting every day, but I am really enjoying it, and would recommend doing a PhD to any interested radiographers. It is hard work, but ultimately, we advance ourselves, our profession and generate evidence for better clinical practice - so a win for everyone.
What made you want to become a radiographer?
I will admit I initially applied to study physiotherapy at uni – but didn’t get the required three A grades during my A level resits.
So my mum gave me the ultimatum of either finding a job or picking another course! She very patiently helped me plough through lots of different course options until I found diagnostic radiography.
I went for a visit to a radiography department for a few hours, and really enjoyed myself. The people were super friendly and it seemed like an interesting career to go into. I have to admit I had never even heard about the radiography profession before this point.
I got a place through clearing at University of Hertfordshire and I've never regretted it since. I am very lucky to have such a wise and patient mum, and a great supporting family behind me.
I even married another radiographer, though we met randomly at an art exhibition in London. It turned out that he knew a radiographer I worked with – it’s a small profession sometimes!
What, for you, are the best parts of being a radiography professional?
I love the variety a day can bring you, and how much the profession has evolved in the 20-plus years I have been in it.
I often have the opportunity to present at multi professional meetings and charity events and I always introduce myself as a diagnostic radiographer to help promote the profession, and hopefully help inspire people to look at it as a career choice.
What developments would you like to see over the next five years in radiography and public health?
For me assessing competency of qualified staff within clinical settings, both initially and ongoing, is definitely a big area we don’t give enough importance to.
I think this is changing and have been really glad to see practice educator roles within trusts appearing, especially in London.
That may be controversial for some, but for me I want to learn from someone I know does it correctly (and has been assessed to show that – not just by an essay) and then know I am also doing it correctly once trained and ongoing.
I really feel that the ‘see one, do one and then teach one’ for all should be a thing of the past.
Sustainability reviews in services would also be great, as I am sure that there are lots of little things that if done by all overall will make an impact.
Can you tell us a bit about your work in CT colonography?
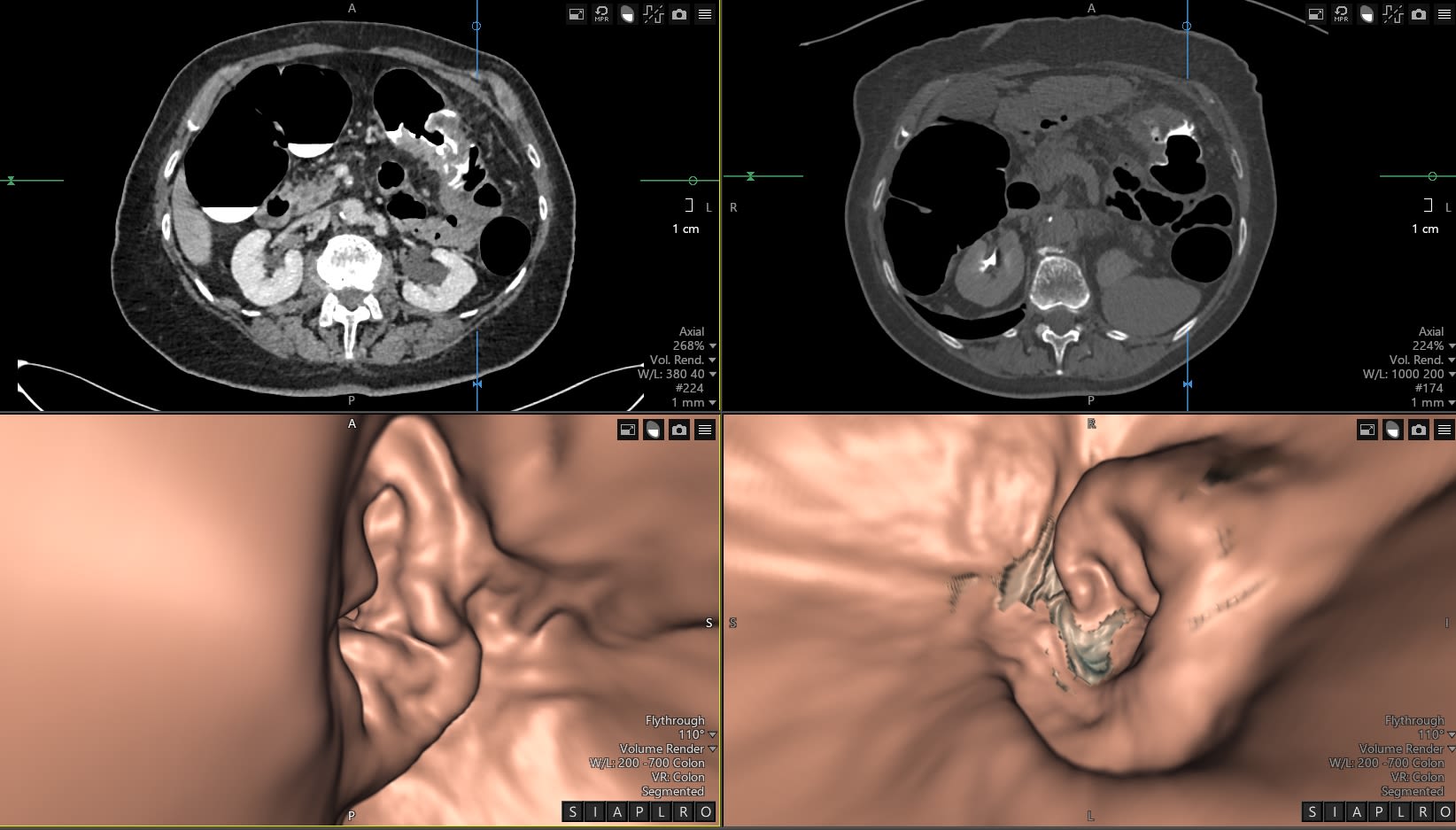
CT colonography is highly sensitive for detecting colorectal cancer and polyps, although reporter competency has a major influence on test accuracy.
There are increasing demands to grow CTC capacity, exasperated by backlogs due to the Covid pandemic, the fall over of lots of endoscopy departments trying to deal with an increase in early onset of colorectal cancer diagnosis and the imminent increase to screening with Lynch syndrome screening coming under the fold of the Bowel Cancer Screening Programme.
This then has the knock-on effect of the need to expand and train the workforce, both to acquire and subsequently interpret CTC. Given the current chronic shortage of radiologists in the UK, there is significant interest in up-skilling radiographers to interpret as well as acquire CTC.
Research has shown that if the test is not performed well to recommended guidelines, and the person reporting it is not well trained, then pathology is missed which ultimately is detrimental to patient outcomes.
CT Colonography scan supine and prone views - showing a large circumferential transverse colon cancer
CT Colonography scan supine and prone views - showing a large circumferential transverse colon cancer
While CTC training programmes have been available in the UK since 2007, there is currently no compulsory national training program, competency testing or accreditation for radiographers or radiologists.
Survey data however suggests a reasonable number of hospitals already currently use radiographers to interpret the colonic portion of CTC, most undertaking a PgCert at a small number of universities hosting CTC courses.
Previous research (PERFECTS study) showed wide variation in current CTC reporting radiologist’s diagnostic accuracy, and although a single day of individualised CTC reporting training supplemented with verbal and written feedback improved performance, up to a third of radiologists were unable to reach adequate sensitivity for pathology. Such data is not available for radiographer reporting, and multi-centre trial data to test how well radiographers respond to training and subsequently perform compared to radiologists is lacking.
The National CT Colonography Training and Accreditation Programme was established in 2020 with the aim to enhance the quality and quantity of CTC in the NHS.
By creating and delivering a new style of training and an assessment programme, in a combination of online and practical methods, the intentions are to improve patient experience, examination safety, efficiency, and capacity to help narrow the wide variation in CTC performance.
Radiographers and radiologists train alongside each other with the same curriculum, which is quite unique in the UK.
Migration from ‘face to face’ to ‘online’ training for reporting CTC will hopefully increase available resources and enable more people to be trained and decrease inequality between people training in CTC reporting.
The aim of my PhD is to understand training, practice and experience of radiographers reporting CTC already, and evaluate new training methodologies for CTC in technique and interpretation.
The PERFECTS-2 study, which is already open, will establish if educational interventions in interpretation make a difference to practise, and confirming if radiographers training can interpret CTC to the same level as training Radiologists.
I hope the impact of my research on healthcare services and patients will be increased utilisation of radiographers for CTC interpretation, as well as improving and speeding up diagnostic result times for patients as a direct result of evidence-based research.
If we help improve and maintain accuracy of reporters, less colorectal cancers and polyps (the precursors) are missed, resulting in less anguish to patients and financial impact to the NHS.
I also hope that it will increase the influence and raise the profile of UK radiographers nationally and internationally, helping career progression and producing a positive effect on radiographic cultures with an associated rise in staff engagement, recruitment, and retention.
Find out more...
Do you have a story to share with fellow radiographers? From promotions to personal achievements and awards, Synergy wants to hear from you.
Members can now submit articles, news stories, research and ideas for content that they would like to see published in the SoR's media outlets by using a single online form, or by emailing the team directly.
Content ideas on all aspects of life as a radiographer are welcome, from service delivery to professional development, to getting recognition for inspiring individuals and pioneering teams.
So if you have a story to tell, get in contact with Synergy today.
There are a number of ways you can get involved with Synergy - you can submit your stories via our member submission portal here.
Just send us a brief description of your story and your contact details, and we’ll be in touch.
Alternatively, if you’d like to discuss your idea with someone from the Synergy team, email synergynews@haymarket.com and we’d be happy to explore your idea.
Image credits:
megaflopp, iStock / Getty Images Plus
zlikovec, iStock / Getty Images Plus