Professional
Sharing knowledge across
the globe
Reporting radiographer Leah Fenning describes her life-changing teaching and learning experience in Uganda with Health Education England
The Gulu Diagnostic Imaging Project (GDIP), run by Health Education England (HEE), was developed to support capacity building in the imaging services of two hospitals in Gulu, a city in the north of Uganda.
The project was co-designed and developed by HEE and key stakeholders, including the overseas partners, between February 2020 and January 2021. The aim was to provide opportunities for NHS staff with imaging expertise to participate in global learning opportunities and to support the development of imaging services at Gulu Regional Referral Hospital and St Mary’s Hospital Lacor. This two-week skills project was developed in response to a request from the overseas partner for face-to-face teaching in radiology.
Since I qualified as a reporting radiographer, a significant part of my role has been training and educating healthcare professionals. This has included teaching on various postgraduate reporting programmes, as well as working with different staff groups from radiology and wider disciplines.
Value of face-to-face interaction
While the pandemic led us to explore the many benefits of online learning, the value of face-to-face interaction and synchronous learning should never be underestimated. Volunteering on the GDIP afforded me the opportunity to combine my enthusiasm for teaching with developing practice in a healthcare setting that would be alien to most radiographers in today’s NHS.
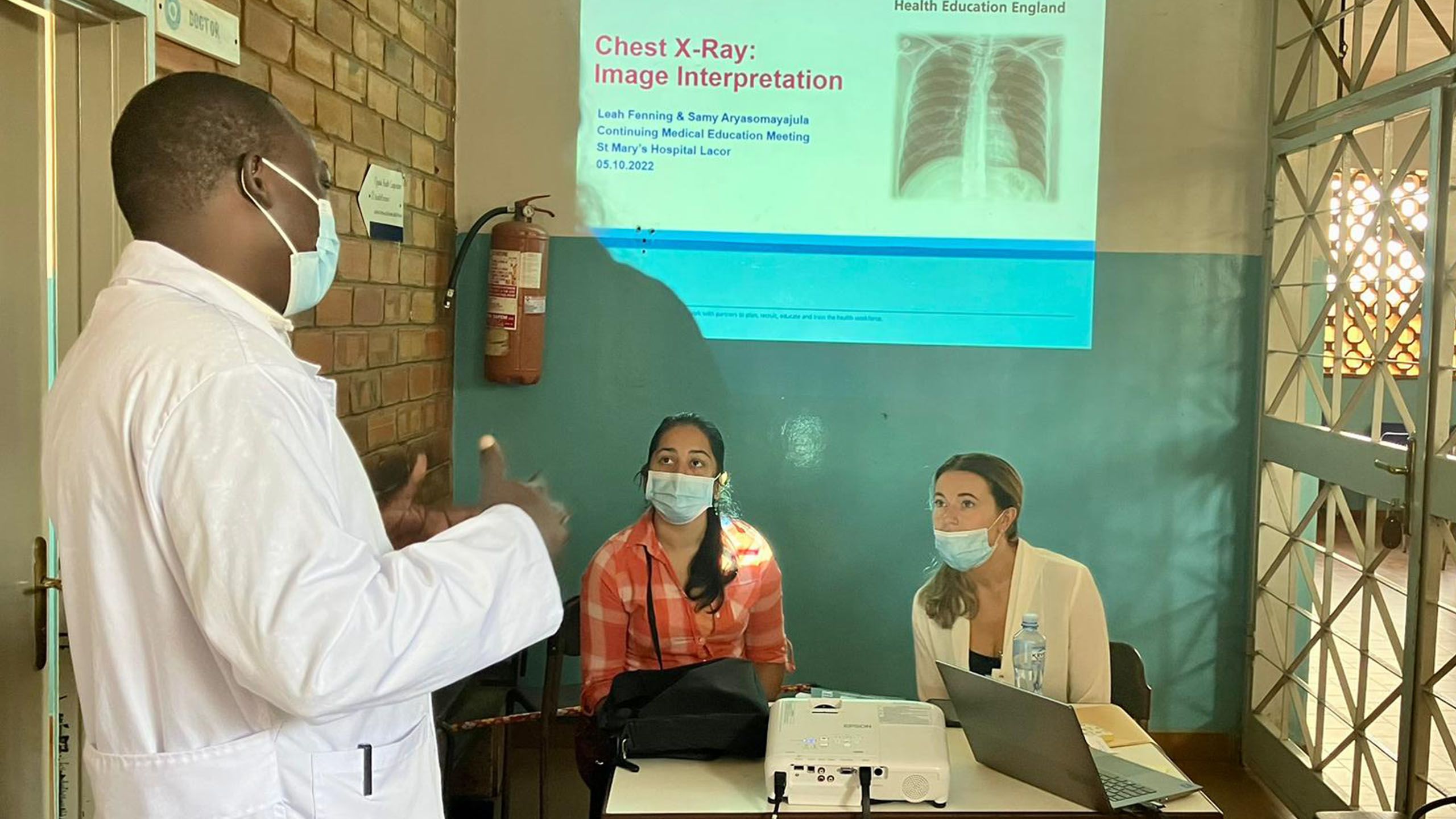
Leah (right) and colleague teaching chest X-ray interpretation
Leah (right) and colleague teaching chest X-ray interpretation
The coordination of training from the UK was challenging and therefore much of the final planning was undertaken while in Uganda. After arriving in the capital city, Kampala, we were welcomed by Joe Bwambale, the President of the Society of Radiographers for Uganda. In our discussions about the project, he explained the need for consistency and standardisation with regards to imaging protocols across the country and we explored the possibility of creating an online community of virtual volunteers to support the project.
After spending just one day at St Mary’s Hospital Lacor, it dawned on me how fortunate we are in the UK. Seeing families camped out in the hospital grounds made a lasting impression on me. It was explained that it is normal practice for hospital patients to be washed and fed by their families because nurses only provide limited levels of care, such as dispensing medication.
Uganda’s healthcare system works on a referral basis relating to levels of severity and complexity. While the government provides some healthcare services for free, other services and treatment require patients to pay. Against the backdrop of the country’s challenging social and economic factors, I witnessed at first hand the consequences and limitations this placed on some Ugandans.
Family camping outside hospital to care for relatives being treated
Family camping outside hospital to care for relatives being treated
Prices for operations listed on the hospital wall
Prices for operations listed on the hospital wall
I was joined on the two-week skills trip by a radiology registrar, who delivered ultrasound training while I focused on X-ray image interpretation. In Gulu, radiology examinations were not reported on because of a lack of radiologists. Accordingly, it was appropriate to focus my efforts on those referrers who were solely responsible for reviewing images.
Our two weeks of skills training complemented the project by supporting a small number of long-term volunteers, who were predominantly working with radiographers to improve image quality. Together we managed to deliver training in ultrasound and image interpretation to more than 150 participants across 24 sessions.
The sessions took a variety of forms, from case-based learning in an outpatient clinic to bi-weekly medical learning meetings with up to 30 staff from different departments. Staff were assessed before and after training to gauge their progress. During the second week, we established connections with the local university and delivered teaching to the medical students on intensive care, with a specific focus on musculoskeletal trauma and chest X-ray interpretation.
Demonstrating ultrasound examinations
Demonstrating ultrasound examinations
I learned a great deal from my experience, particularly about the diseases prevalent in Uganda, such as sickle cell disease and tuberculosis, which are less commonly seen in my own practice.
Staff shortage and clinical demands
While many of the challenges were unique to Africa, many were similar to those experienced in the UK, for example, a workforce shortage in terms of capacity and capability. The competing demands of clinical staff in the outpatient department meant it was not always possible for them to attend theory sessions delivered through the GDIP. There was no appointment system so, if patients were not seen, they simply returned the next day in the hope that a doctor would be available.
The staff shortage, coupled with clinical demands, often meant the start of our planned training was delayed. I quickly became accustomed to “Africa time”, a cultural tendency whereby time is more relaxed than regulated. Consequently, staff often arrived later than scheduled. Initially, this was difficult to comprehend but I soon discovered that some staff had other jobs, such as working in the local market, to ensure they could provide for their families because wages were not always paid on time by the government.
Supporting a local business by commissioning a traditional outfit
Supporting a local business by commissioning a traditional outfit
A warm and friendly community
I now appreciate why Uganda is often considered the friendliest African nation and a place with customs, cultures and communities that can be navigated with ease. I was fortunate to be there for Independence Day and felt the warmth of the people and an overriding sense of community. I was made extremely welcome and I immersed myself in local experiences. This included taking a local bus ride, trips to the main market and trying the most famous local delicacy, the vegetable malakwang. A local resident in Gulu made me a traditional outfit and it was great to be able to support a local business. My love for Liverpool FC was reciprocated and it felt appropriate to present a club scarf to Denis, one of the staff who made sure we felt safe throughout our stay.
Sharing the love for Liverpool FC
Sharing the love for Liverpool FC
By the end of the trip, intermittent power cuts, late starts and faulty projectors became the norm. Although this was challenging, it has definitely given me more resilience in dealing with limited resources and being innovative in addressing problems. It has also increased my overall professional satisfaction and helped me identify my future career path in the NHS.
Our time in Gulu was highly valued by the overseas partner and, since we returned to the UK, an agreement has been reached to continue mentoring our Ugandan colleagues. I continue to maintain relationships in Gulu and deliver monthly online sessions to the medical students.
My time volunteering was one of the most meaningful experiences, both personally and professionally. I would have no hesitation in recommending the GDIP to any radiographer interested in service improvement. Even in this short period of time, I learned so much and returned with a new appreciation for the quality of healthcare in the UK.
About
Leah Fenning is a reporting radiographer at Wrightington, Wigan and Leigh Teaching Hospitals NHS Trust.
Find out more
To discover more about the Gulu Diagnostic Imaging Project and other global learning opportunities, visit the Health Education England website.
Images credit Leah Fenning
Now read...