Professional
Time to lead on cancer research
Therapeutic radiographers are taking their place at the forefront of patient-centred cancer research

Will Kinnaird
Will Kinnaird
Self-reliant, determined and uncomplaining – my grandma was typical of the wartime generation. Nana Grimsby, as we called her, barely mentioned the arm that hung limp by her side. The only time it was referenced was under her breath as she heaved its weight onto the table at teatime. “Come on thingy”, she would mutter.
Nana Grimsby had suffered the debilitating effects of brutal 1950s radiotherapy for breast cancer when aged just 36. It saved her life but left her with severe lymphoedema in her left arm that eventually led to the loss of all function and feeling.
She was offered an amputation but decided it would be more useful to keep the limb. She would wedge a jam jar into her armpit to help twist off the lid or use it as a counterweight when chopping food. But it also meant living with pain in her shoulder and she would cut or burn herself without noticing.
Nana Grimsby was treated in an era where clinical efficacy was the sole measure of success. Only a minority of people survived cancer, so the main aim was to find a cure, whatever the cost.

Helen McNair
Helen McNair
New focus on patient experience
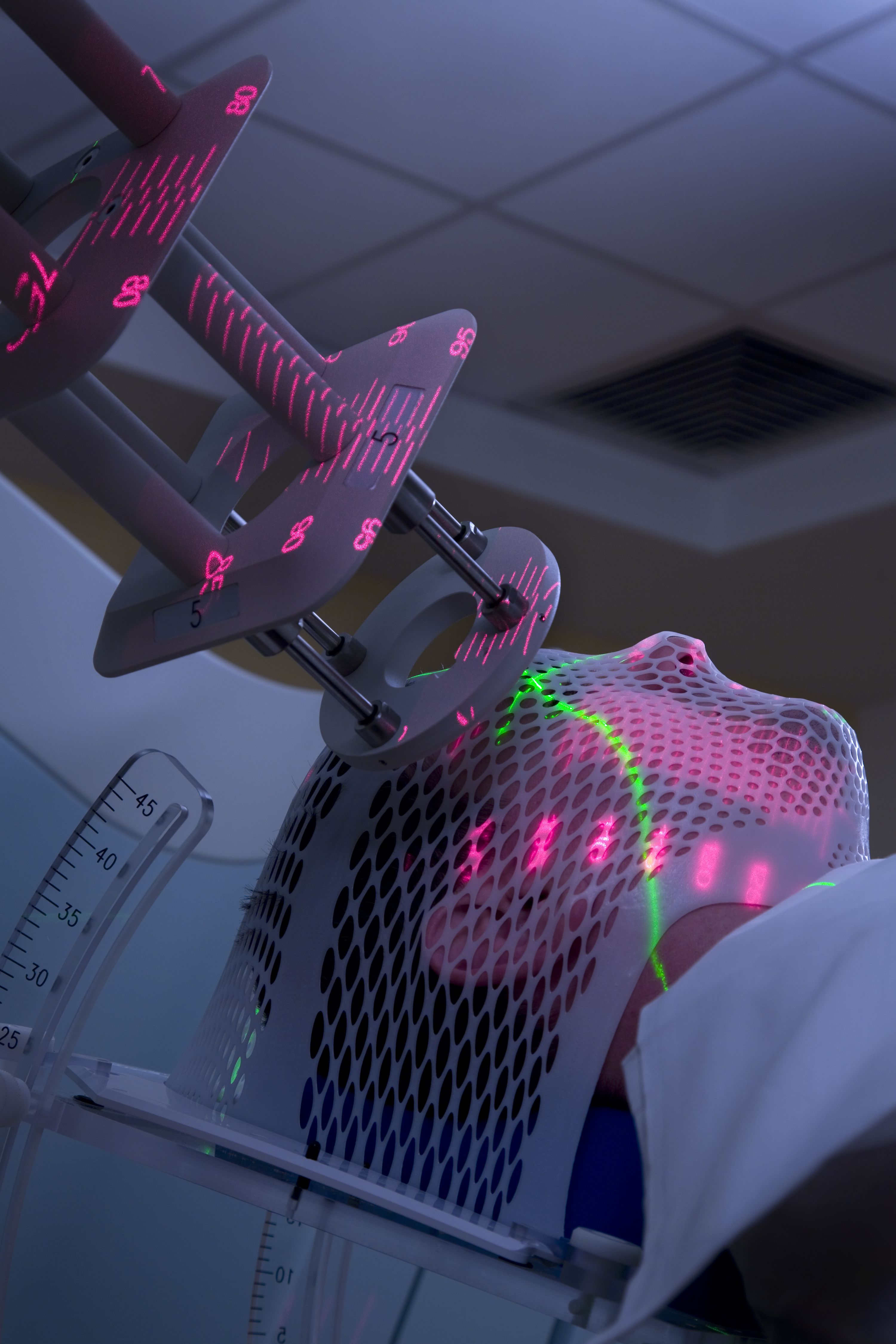
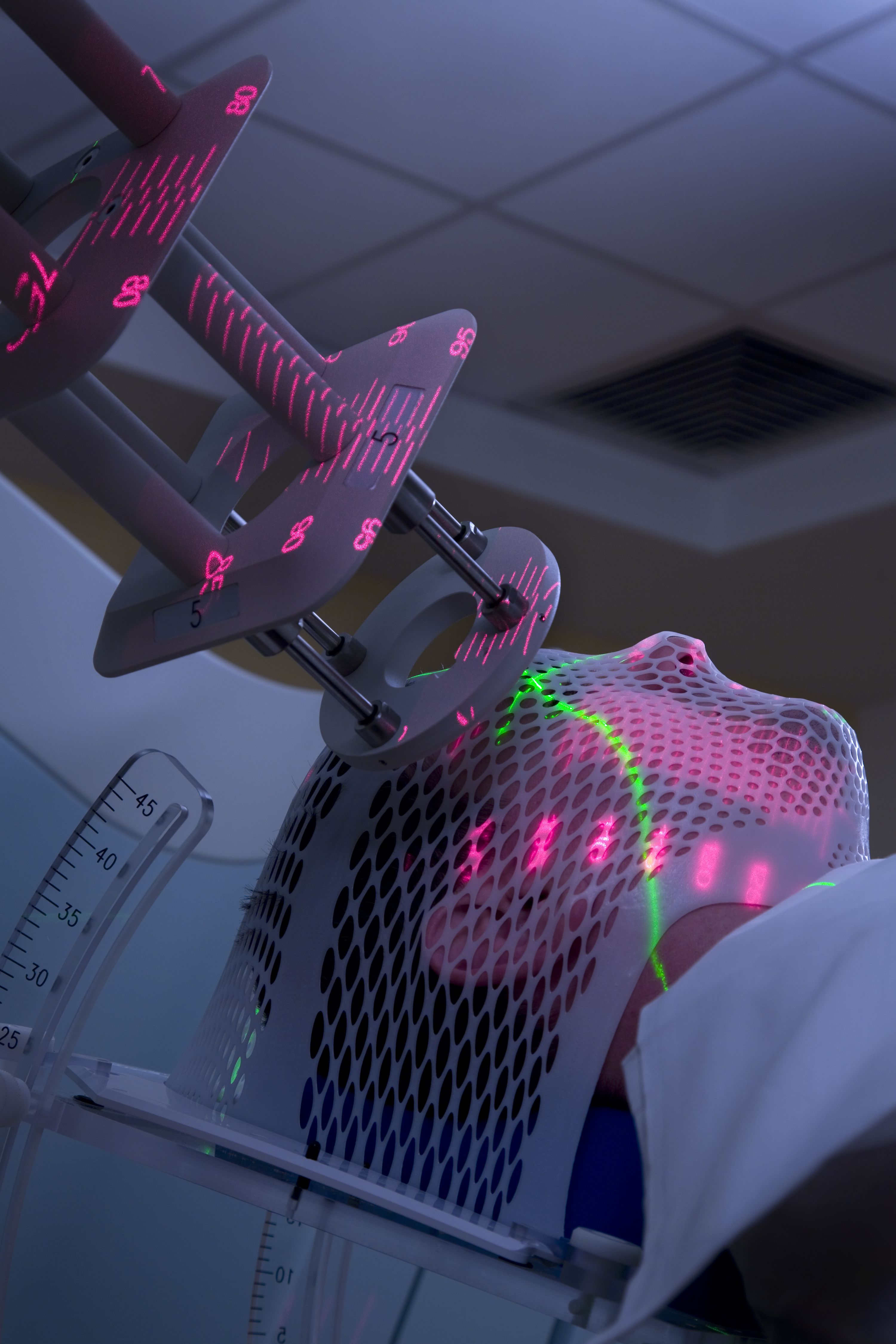
Radiotherapy has come a long way from the crude treatment fields of the 1950s, with sophisticated image-guided treatment offering sub-millimetre accuracy. This means, for many in oncology, that the focus has shifted towards the patient experience. With rising life expectancy, there is a growing movement to ensure that improvements in survival are matched by improvements in quality of life.
It’s precisely this area where therapeutic radiographers are often found focusing their efforts, according to Dr Helen McNair, lead research radiographer at the Royal Marsden Hospital and reader in translational therapeutic radiography at The Institute of Cancer Research.
“We’re the only profession that delivers radiotherapy”, she said. “So we’ve got that day-to-day contact with the patient and we’re best placed to identify what the patient needs and the impact of changes on them. We see not only the treatment but also how the patient interacts with it.
“The focus of research is on improving patient outcomes but it’s not all about survival. It is also about how the patient experiences that survival. Living with and beyond cancer is their experience of treatment. And if we can make that better, then surely that’s improving patient outcome.”
Where theory meets practice
Having worked in research for more than two decades, Dr McNair has seen therapeutic radiographers start to carve a niche in the area where theory meets practice.
Her own research has focused on the translation of new radiotherapy technologies into clinical practice, including the introduction of MR-based radiotherapy treatment. She believes there is a bond that builds between the patient and therapeutic radiographer over days, weeks and sometimes months of radiotherapy treatment, which brings a deeper understanding.
“I think we’re pretty good at that,” she said. “The research we do is very much driven by the patient and what the patient needs. I really do believe that. One of the benefits of being clinical and doing research is that we’re in touch with what’s happening. We know what changes are coming in terms of technology or trial design and we want to understand the impact they might have on the patient. We’re ready to answer those questions.”

Dr Rachel Harris
Dr Rachel Harris
Her views are echoed by Dr Rachel Harris, head of professional practice and education at the Society and College of Radiographers (SoR | CoR), who has led research on managing radiation-induced skin reactions.
“Therapeutic radiographers like looking at the qualitative aspects as well as the technical side”, she said. “We are quite a unique breed. I can pick out a therapeutic radiographer in a room. We like listening to patients and understanding their experience. We are able to do quantitative research but we are also able to focus on quality of life and patient voice. And I mean true patient voice and involving patients in research.”
“If there is research being done then it should be led by that staff group”
“We are the only profession that gets into a cancer training environment from day one. No-one else is qualified to operate and use radiotherapy equipment so if there is research being done then it should be led by that staff group,” she said.
“We need clinical practitioners who are leaders to conduct research around radiotherapy. We have to do it as a priority for improving patient care. No other staff group can do it. How can anyone else have the underlying knowledge base? We are the ones who understand treatment.”
A quick PubMed search reveals the number of publications including the word ‘radiographer’ has risen from just over 4,000 per year in 2000 to almost 13,000 in 2022. There are also well over 100 doctorates listed as underway or completed by radiographers on the College of Radiographers website.
A record 564 therapeutic radiographers attended the 2023 European Society for Radiotherapy and Oncology (ESTRO) Congress in May, making up 13.1% of delegates. They showcased a range of technical and translational work, with a particular emphasis on patient experience.
A foothold in research
But for a small profession like therapeutic radiography, with between 4,000 to 5,000 registered professionals in the UK, it has been a long battle to get a foothold in research and academia. In 2022, the first therapeutic radiography doctoral school opened in the UK at University College London (UCL), endorsed by the SoR | CoR, as well as Cancer Research UK.
The project was led by two academic physicists, Professor Andrew Nisbet and Professor Gary Royle, who recognised the unique skills of radiographers and wanted to offer them a platform into research.
“UCL has strong research groups in medicine, physics and engineering, but we have a gap in translating rapidly advancing technologies into evidenced-based benefit for patients”, said Professor Nisbet, head of the UCL Medical Physics and Biomedical Engineering department.
“Because therapeutic radiographers are patient-focused, they are ideally placed to do this research. We believe many radiographers are interested in research, and this programme can help them develop into very successful independent researchers.”

Dr Amy Hancock
Dr Amy Hancock
Academic careers
A growing number of radiographers are now starting to forge academic careers, including Dr Amy Hancock, a therapeutic radiographer and senior lecturer in medical imaging at the University of Exeter.
Amy was part of a multidisciplinary team awarded £3.3m from the NIHR to fund the TOURIST trial focused on assessing the use of palliative radiotherapy and systemic therapies in the treatment of Stage IV Non-Small Cell Lung Cancer.
“Radiographer-led research is definitely growing”, she said. “It’s one of the four pillars of advanced practice so there is a requirement for us to be involved. Previously, there has been the perception that radiographers are only involved in clinical trials work, doing the practical aspects of research on behalf of someone else.
“But now there is an expectation and desire to lead our own research. There has always been research going on but often people did not feel it was worth publishing and sharing. It is important for people to publish and get their work out there at conferences.
“There are lots of outlets, including UKIO, ARC, ESTRO, ASTRO, and our own professional journal Radiography. There is funding available from the College of Radiographers Industry Partnership Scheme and doctoral funds, and there are more people than ever with doctorates who are making a path for other radiographers to follow them.”
“Compared with other professions, we are still in the infant stages ”
Progress has not moved fast enough for some, though, and many frontline radiographers complain they are not given the support, training, time and encouragement to get involved in research, which is often the first of the four pillars of advanced practice – clinical practice, leadership, education and research – to be squeezed by staff shortages and heavy workloads.
Dr Yatman Tsang, who recently moved from the UK to be appointed director of radiation therapy at the Princess Margaret Cancer Centre in Toronto, Canada, said the profession needed to really embrace research. He said radiographers had to work hard to establish a research community in order to get a seat at the top table.
“I would compare the situation to a body where we have all the organs but they’re not yet working together properly”, he said. “I feel like we have done a lot of work and we are making a lot of progress but, compared with other professions, we are still in the infant stages. We have a really good cohort, but I think we still need to try to join things together to amplify.”

Danny Hutton
Danny Hutton
The old hierarchy is breaking down
Danny Hutton is programme manager for the North West Radiotherapy Operational Delivery Network, one of eleven regional networks overseeing all aspects of radiotherapy service delivery in England.
His research has focused on patient experience but also the real-world experiences of frontline radiotherapy staff, and he has seen the therapeutic radiographer role develop beyond the traditional planning and treatment elements.
Danny said the expansion of advanced practice and consultant radiographers in the clinical setting was starting to be mirrored in research and trials, and this growing interest in research was making a difference to patient care, with radiographers leading on service development.
“The old hierarchy of doctors, then nurses, then all the other allied health professionals, is changing”, said Danny. “We are seeing more and more radiographers getting involved in research and the boundaries are being blurred.
“The nature of the job means therapeutic radiographers tend to be quite solution-focused. This is reflected in the type of research we carry out, where there is usually an end in mind. For example, there is a growing interest in late effects. We’ve made so many advances with treatment and helping people live longer but sometimes we don’t give enough thought to what happens after treatment.
“Radiographers are increasingly providing that missing piece of the puzzle – and focusing on how we help people live well with cancer.”
It’s an undertaking that grows more important by the day as life expectancy, cancer detection and therapies continue to improve rapidly. Therapeutic radiographers find themselves at the intersection of scientific progress and real-life impact. In the ever-evolving landscape of radiotherapy, they stand as beacons of both innovation and compassion.
And as therapeutic radiographers embrace the challenges and opportunities of research, their commitment to amplifying the patient voice paves the way for a more empathetic, tailored, and effective approach to cancer care.

PhotoQuest / Contributor/ Getty Images
PhotoQuest / Contributor/ Getty Images
Mark Kostich/ Getty Images
Mark Kostich/ Getty Images

SDI Productions/ Getty Images
SDI Productions/ Getty Images

SDI Productions / Getty Images
SDI Productions / Getty Images

vm/ Getty Images
vm/ Getty Images
Find out more...
Will Kinnaird is consultant therapeutic radiographer at UCLH NHS Foundation Trust and a doctoral researcher at University College London.
The College of Radiographers is supporting an NIHR-funded
incubator for the development of diagnostic and therapeutic
radiographer research. The steering group is conducting a survey to better understand the research culture in the radiography workplace, and identify barriers and enablers for radiographers to be involved in and lead research. Please click here to complete the survey or scan the QR code.
This article was first published by Cancer Research UK (CRUK). For researchers exploring issues in cancer science, check out more articles and podcasts issues from CRUK here.
Scan or click the QR code to find out more
Scan or click the QR code to find out more
Now read...