The evolving radiographer: how the profession has undergone revolutionary change in the past 30 years
The role of a radiographer has undergone dramatic change in recent decades. Marese O’Hagan explores the driving factors behind the shift and what the job could look like in the future

By Marese O’Hagan, senior reporter
By Marese O’Hagan, senior reporter
The role of a radiographer has undergone huge change since the discovery of X-rays in 1895. With its origins in Wilhelm Röntgen’s revolutionary discovery 130 years ago, radiography has developed from a new technique used by various health workers into its own profession, complete with regulation and protected titles from the Health and Care Professions Council.
Both Diagnostic and Therapeutic Radiographers now take on increased responsibility in an ever-expanding scope of practice. From the rapid acceleration of technological advancement in imaging to staff shortages necessitating change, modern radiography is unrecognisable from its early form.
But how exactly has the profession changed in recent years? Synergy delves into the history of the role and how it has evolved since its inception.
By Marese O’Hagan, senior reporter
By Marese O’Hagan, senior reporter
The role of a radiographer has undergone huge change since the discovery of X-rays in 1895. With its origins in Wilhelm Röntgen’s revolutionary discovery 130 years ago, radiography has developed from a new technique used by various health workers into its own profession, complete with regulation and protected titles from the Health and Care Professions Council.
Both Diagnostic and Therapeutic Radiographers now take on increased responsibility in an ever-expanding scope of practice. From the rapid acceleration of technological advancement in imaging to staff shortages necessitating change, modern radiography is unrecognisable from its early form.
But how exactly has the profession changed in recent years? Synergy delves into the history of the role and how it has evolved since its inception.

More responsibility, more recognition
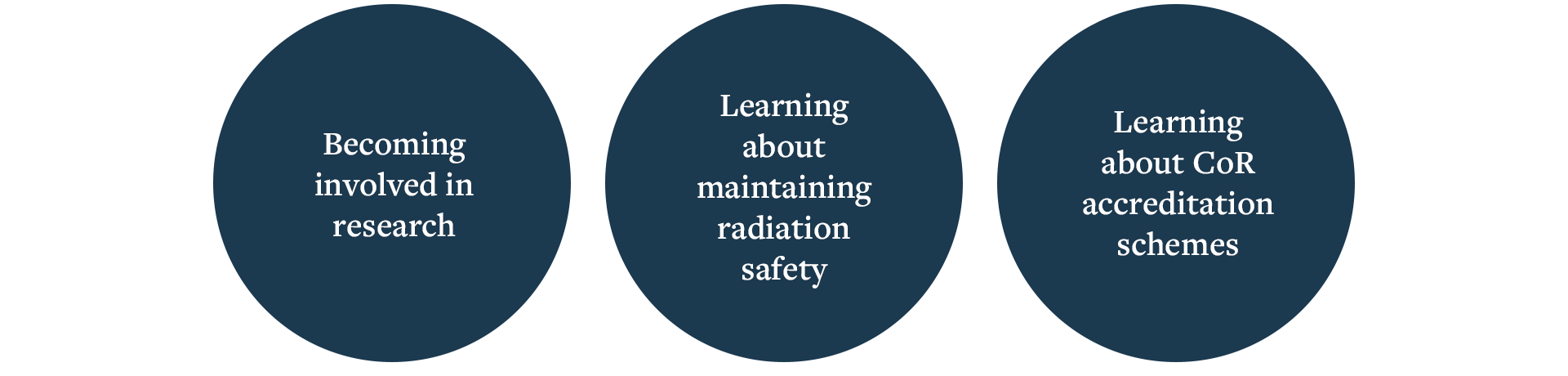
Morag Stout is a clinical lead at NHS Scotland Academy’s National US Training Programme. Having qualified as a sonographer in 1998 and progressed to a consultant role, Morag has seen firsthand how radiographers have been able to expand their responsibilities. “The role of the radiographer has evolved enormously since I qualified,” says Morag. “There are more opportunities to develop clinical roles in multiple subspecialities and opportunities to work in practice education, education and research.
“Pertinently, these involve more responsibility. I think the profession is now more recognised and respected nationally.”
Opportunities for greater autonomy and more senior roles are also changes that Jancis Kinsman has seen throughout her career. Jancis is an accredited advanced practitioner with the Centre for Advancing Practice and has had a front-row seat to the advances in the profession, having been a Therapeutic Radiographer for more than 30 years. Working as a lung specialist, image-guided radiotherapy and stereotactic ablative radiotherapy lead radiographer at the Bristol Cancer Institute, Jancis says radiographers are much more autonomous now compared to when she first started working, owing in part to a shortage in clinical oncologists.
Radiographers have stepped up to the plate, she says: “Radiographers have embraced the opportunities to expand their roles with prescribing and management of toxicities, image review and advanced roles where they may be responsible for the entire radiotherapy pathway, consenting patients for treatment, marking radiotherapy volumes and prescribing treatment and following patients up afterwards.”
History of the role of the radiographer
It is well known that the history of radiography starts with the discovery of X-rays by Röntgen in 1895. From that watershed moment, medical imaging was quickly adopted within a few short months and was soon being utilised on European battlefields during conflicts in the early part of the 20th century, as X-rays were used to locate bullets and shrapnel in the bodies of wounded soldiers.
Alongside diagnostic imaging, radiography was also quickly utilised for the treatment of cancer, with the first recorded use of radiation for this dating back to 1896.
Early in the history of radiography, scans were carried out by various professionals, from physicians to physicists and even photographers. But in the decades that followed, and as the risks that came with the use of radiation for imaging became clear, there was an increasing need for highly trained and regulated professionals to carry out scans.
In one tragic incident in 1929, an eight-year-old child died in an electrical accident, believed to have been caused when a nurse inadvertently created an electric circuit from high-tension cables through to the child. This incident saw a coroner later conclude that hospitals should reconsider allowing inexperienced individuals into X-ray rooms. There were also worries surrounding radiation and the potential for injury among staff and patients.
This risk of injury and the lack of training for operators of X-ray equipment resulted in the need for qualified radiography professionals, and the first qualified radiographers began to take up their positions in the 1920s. Alongside the emergence of radiography roles, the Society of Radiographers was established in 1920 to provide a profession-wide standard for care, professionalism and treatment. It is one of the oldest radiography societies in the world.
Diversifying the role
Melanie Clarkson is a senior lecturer in radiotherapy and oncology at Sheffield Hallam University and leads the accredited MSc Advanced Clinical Practice Radiotherapy and Oncology programme. Melanie has also championed the Society and College’s work on enhanced and advanced practice. In addition, in her role supervising advanced practitioners via the Centre for Advancing Practice’s ePortfolio Route, she has seen firsthand how radiography education has had to adapt with the ever-changing demands of the profession.
From Melanie’s perspective, over the years an increased awareness of the ‘four pillars’ has helped to improve the visibility of radiographers across different aspects of the role. The society and college first adopted the four pillars of practice within its Education and Career Framework for Radiographers (ECF) from 2006 onwards. The four pillars are a golden thread across all levels and roles included in the most recent iteration, published in 2022.
The four pillars, highlighted in the multi-professional advanced practice framework and the ECF fourth edition, support the evolution and development of radiographers working at an advancing practice level, consisting of clinical practice, education, leadership and management, and research and development. “I think previously [radiographers] often felt very stuck – that the only thing we could do was to either run up and down the room to treat a patient or, equally, in imaging, to run in and out of the room to take the image,” Melanie tells Synergy.
“But I think there are opportunities for us to diversify our roles because of the four pillars, and to be more innovative and actually have a system impact, depending on the level of practice we work at, where we can change practice and services and we haven’t got the monotony of the past.”
Advanced practice first emerged within the NHS in the 1970s, giving healthcare professionals the opportunity to expand their expertise within their field, taking the four pillars as the basis for that career development. As a growing area within radiography, advanced practice presents an opportunity for radiographers to take on more responsibility and increased autonomy.
That wider impact is a sentiment echoed by Jancis, who has personally been involved in developing radiographer prescribing for a number of years, and also chairs the SoR’s Supply, Administration and Prescribing of Medicines SIG. “Role expansion offers opportunities to diversify and specialise that are important for the recruitment and retention of the workforce,” she says.
Take the opportunity
Despite ongoing pressures and constraints within the NHS, radiographers are still taking opportunities to diversify their roles. Sabina Khan is a consultant head and neck Therapeutic Radiographer with a focus on late effects and an advanced practitioner with the Centre for Advancing Practice, adding another string to her bow. She describes the accreditation as “formal recognition for the work I’ve been doing over the last decade”.
Sabina says she believes that radiographers who decide to pursue specialisation should be supported, particularly within advanced practice. However, she adds that this needs to be done carefully. “It’s vital that we support individuals who see specialisation as a key component of their career development and a pathway to fulfilling all four pillars of advanced practice,” she says. “However, it’s equally important to recognise that ‘advancing practice’ is relevant to every role within radiotherapy.
“Continuous development empowers us to become better healthcare professionals, fosters role progression and enhances job satisfaction – regardless of our position. That said, this growth must be pursued safely, with robust support systems embedded within our teams to ensure sustainability and wellbeing.”
Gillian Thomas is a consultant radiographer working in brachytherapy at Poole Hospital. For her, the skills that inherently come with practising radiography make it the ideal profession for role expansion. “Radiographers have vast experience and knowledge that can be focused to develop roles and gain responsibilities,” she explains. “Not only is this good career progression, it is also attractive to the recruitment to the role.
“By expanding their role, radiographers gains recognition in other professions. So if radiographers do not get involved in role expansion, we will get left behind and be underrepresented.”
The public perception
Although nine out of 10 NHS patients will see a radiographer at some point throughout their patient pathway, there is still a gap in public understanding of the role of radiographer. When a radiographer’s responsibilities are expanded, this can cause further confusion, Gillian says. “Within the local services, I would say it is received positively as some role expansion frees up consultant time, for example,” she explains. “This means they get the direct benefit of this.
“I imagine it can also cause some conflict if some role expansion extends to something similar to what a specialist nurse currently does, so they may feel threatened. Widely with the public, however, radiographers’ roles are still largely unknown.”
Liz West, an advanced clinical practitioner in palliative radiotherapy, says she has experienced first-hand the effects of these blurred lines as her career saw her take on more responsibilities. “When I started doing different things, it was quite difficult in some respects,” she tells Synergy. “People say ‘well, you’re not a nurse’ but I can still do these things. It’s people jumping out of their boxes and perhaps trying to take on responsibilities that have traditionally been for other people.”
But these issues can be worked through when people are given time to adjust, she adds: “There is a bit of resistance. I think traditionally medicine is quite hierarchical. It takes a little time to get over that, the traditional boundaries. Generally speaking, I think it’s quite well received.”
Supporting radiographers to expand their roles
In its role as a professional body and trade union, the SoR offers various resources to support the career development of its members. Central to this work is the ECF, the fourth edition of which was published in 2022 and which offers guidance and career development for the radiography profession. It is aligned with policy across England, Scotland, Wales and Northern Ireland and aims to guide radiographers through the various career and educational pathways.
The ECF can be used by members for a number of outcomes, including:
Charlotte Beardmore, the SoR’s executive director for professional policy, says SoR frameworks like the ECF give clear guidance to members about what they can expect when working across different positions. “We are very mindful of emerging advanced practice frameworks that exist, such as the multi-professional framework for advanced level practice in England, and similar in the devolved nations of the UK,” she says. “Our frameworks articulate and deliver our expectations for the profession working at those different levels.”
Charlotte explains that the framework offers guidance and advice for radiography roles beyond the practitioner level, into enhanced, advanced and consultant levels of radiography practice. “We also need to acknowledge that there are wider roles in academia, education, research and service leadership, all of which are encompassed within this framework,” she continues. “This is the backbone to support those different areas – those different levels of practice.”
Kathryn Williamson, professional officer for education and accreditation for the College of Radiographers, describes the ECF as an “education and career roadmap for the entire radiography workforce”.
“It covers the educational expectations and the scope of practice expectations, as well as the four pillars of practice and the knowledge, skills and attributes expected across all different levels of practice, including the support workforce right through to consultant-level practitioners,” she explains.
What next?
It could be said that radiography as a profession is in one of the most turbulent times of change in its history. In the UK government’s Change NHS 10 Year Health Plan, prime minister Keir Starmer vowed to improve the health service by focusing on three main measures: shifting care from hospitals to communities, improving the use of technology and preventing sickness.
While there have been successes – including more than two million extra NHS appointments being delivered ahead of schedule – the Society of Radiographers has warned that the radiography workforce will need continued investment to keep up with demand.
Paired with the unexpected announcement earlier this year of the abolition of NHS England, 2025 has been a stressful and uncertain time to work in the health service.
Liz West believes that, in the future, radiographers can expect to have more opportunities to specialise and refine their skills, as well as see more regulation. “There’ll be more opportunities to specialise,” she says. “I think it’ll be easier to do things like non-medical prescribing without having to jump through hoops to do it.”
Kathryn Williamson says the ECF will continue to act as an anchor for those moving into advanced practice. “The Education and Career Framework is intended to support both the current and future development of the radiography profession, including those progressing into advancing practice,” she explains. “To support practitioners through the increasing levels of risk and complexity associated with advancing practice it is key that those working at these levels have the appropriate underpinning education and training to fulfil the expectations of their role safely and effectively.
“The ECF can support individual practitioners, service managers and our radiography academic workforce to meet their responsibilities regarding education and training needs.”
For Morag Stout, continuous role development – specifically in imaging, intervention and reporting – into the future is vital to keep meeting demand. “We must increase numbers of practice educators to accommodate this [increasing demand],” she says. “Continued collaboration between clinical colleagues and industry – particularly around AI – is necessary.”
Sabina Khan believes that Therapeutic Radiographers have consistently adapted to the increasing pressures and lack of resources afflicted upon the NHS, and sees them as ideal examples evolving under pressure. “Their contributions now extend beyond imaging and treatment to include patient education, pathway redesign and service development, all aimed at improving outcomes and delivering more personalised care,” she says.
The radiography profession has evolved significantly since X-rays were discovered. Today, there are more opportunities than ever for radiographers to simultaneously broaden their career horizons and help to improve standards of care. It is this balance that encapsulates the development of the radiographer role, Charlotte Beardmore concludes.
“Overall, the profession has been really keen to develop,” Charlotte remarks. “We are all human. We want to ensure that we're doing the right things for patients, the best things we can, but we also want to improve and we want career development.”
What next?
It could be said that radiography as a profession is in one of the most turbulent times of change in its history. In the UK government’s Change NHS 10 Year Health Plan, prime minister Keir Starmer vowed to improve the health service by focusing on three main measures: shifting care from hospitals to communities, improving the use of technology and preventing sickness.
While there have been successes – including more than two million extra NHS appointments being delivered ahead of schedule – the Society of Radiographers has warned that the radiography workforce will need continued investment to keep up with demand.
Paired with the unexpected announcement earlier this year of the abolition of NHS England, 2025 has been a stressful and uncertain time to work in the health service.
Liz West believes that, in the future, radiographers can expect to have more opportunities to specialise and refine their skills, as well as see more regulation. “There’ll be more opportunities to specialise,” she says. “I think it’ll be easier to do things like non-medical prescribing without having to jump through hoops of fire to do it.”
Kathryn Williamson says the ECF will continue to act as an anchor for those moving into advanced practice. “The Education and Career Framework is intended to support both the current and future development of the radiography profession, including those progressing into advancing practice,” she explains. “To support practitioners through the increasing levels of risk and complexity associated with advancing practice it is key that those working at these levels have the appropriate underpinning education and training to fulfil the expectations of their role safely and effectively.
“The ECF can support individual practitioners, service managers and our radiography academic workforce to meet their responsibilities regarding education and training needs.”
For Morag Stout, continuous role development – specifically in imaging, intervention and reporting – into the future is vital to keep meeting demand. “We must increase numbers of practice educators to accommodate this [increasing demand],” she says. “Continued collaboration between clinical colleagues and industry – particularly around AI – is necessary.”
Sabina Khan believes that Therapeutic Radiographers have consistently adapted to the increasing pressures and lack of resources afflicted upon the NHS, and sees them as ideal examples evolving under pressure. “Their contributions now extend beyond imaging and treatment to include patient education, pathway redesign and service development, all aimed at improving outcomes and delivering more personalised care,” she says.
The radiography profession has evolved significantly since X-rays were discovered. Today, there are more opportunities than ever for radiographers to simultaneously broaden their career horizons and help to improve standards of care. It is this balance that encapsulates the development of the radiographer role, Charlotte Beardmore concludes.
More on support from the SoR
The Society of Radiographers published two documents focusing on scope of practice for members earlier this year: ‘Scope of Practice’ and ‘Guidance on scope of practice for advanced practitioners and consultant practitioners’.
For more information about advancing practice, check out the Advancing Practice in Radiotherapy SIG here.
Image credit: Getty Images
Read more