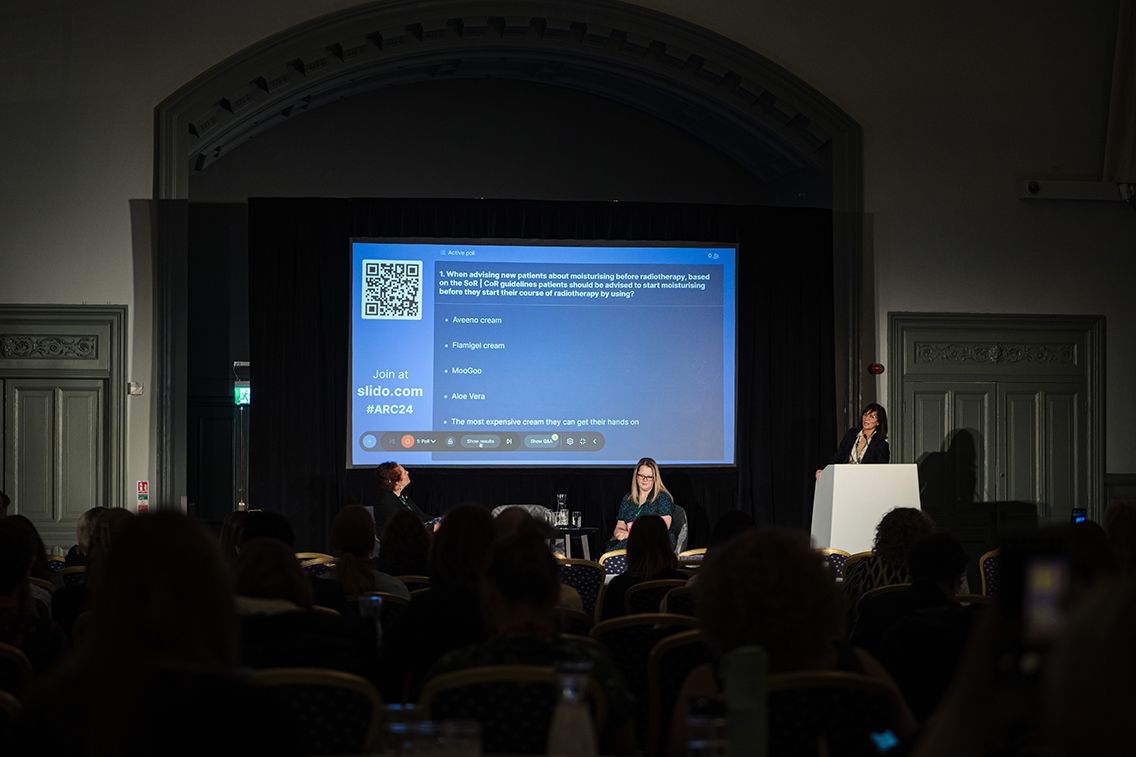
‘Working together for patients’: the Annual Radiotherapy Conference 2024
In October, the Annual Radiotherapy Conference took place for the first time since 2019. Synergy was on hand to report on the return of the successful event
The excitement is palpable in the foyer of the Brighton DoubleTree hotel, as Therapeutic Radiographers prepare to head into the luxurious main conference room.
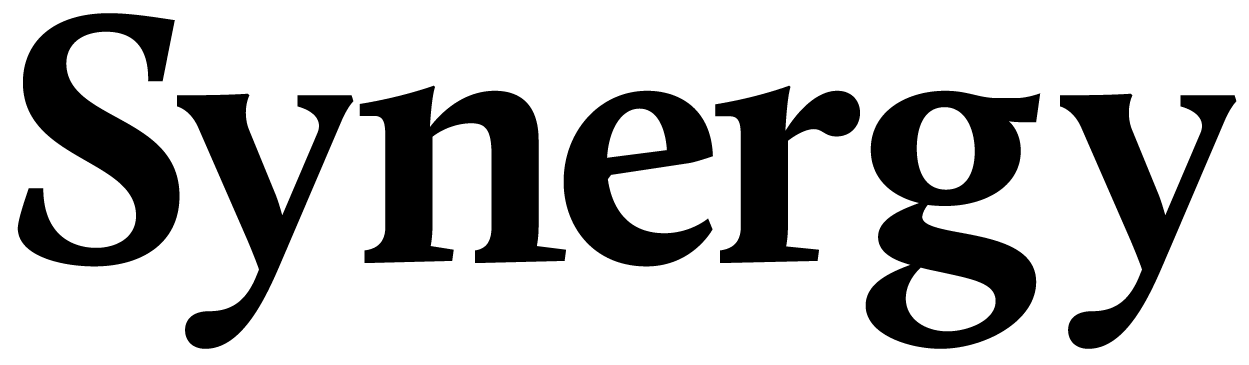
Launching for the first time since before the onset of the pandemic, the Annual Radiotherapy Conference (ARC) took place in Brighton from 4 to 5 October, bringing together experts from across the country for two days of exhibitions, professional development and clinical advancements in everything from the latest technology to advice on person-centred care.
ARC kickstarted with an address from Tom Welton, president of the SoR, and attendees were then given a chance to hear from expert Therapeutic Radiographers, national project leads, clinical oncologists, medical physics staff and radiotherapy service managers on the latest developments and important trends in the profession.
From questions of recruitment and retention to the latest in radiotherapy treatment techniques, a whole range of topics were covered across question and answer sessions, professional presentations and individual breakout rooms.

Day one – person or patient?
ARC 2024 focused on the notion of ‘person-centred care’, as distinguished from simply ‘patient-centred care’. By adopting this concept into your practice, the speakers explained, services can improve the experience of not just their patients, but their radiotherapy teams as well. “If we work together as a team, the patients benefit. Hold on to that patient-centred care,” said Tom.
“To be truly person centred, we need to be willing to improve. The only way to do that is to be true to yourselves and true as radiographers. Make a promise to be true to yourself and make a promise to learn. You’ll learn things over the next couple days that you can put into practice in your departments.”
After ARC’s opening address, audiences heard from Nicky Whilde, head of radiotherapy physics at the Mid and South Essex NHS Foundation Trust, Jo Penman, head of radiotherapy services at the Somerset NHS Foundation Trust, and Nicky Thorp, consultant clinical oncologist at the Christie Hospital NHS Foundation Trust.
“Radiotherapy has always been patient-centred, but we move on. Or do we?” said Nicky. “In 80 years, the model hasn’t changed. Surely there’s a better way of taking care of people? We never get to see the patient afterward. We barely get to know if they live or die. We need to finish the loop – look at the late effects, and see if we can improve the planning.”
Jo, meanwhile, discussed NHS England’s methods for measuring productivity – asking ‘what can you lose?’ and ‘how can we do more for less?’ But these questions are not always conducive to the quality standard of care that radiotherapy requires. Patient numbers are going up, and NHSE money is being thrown at diagnostics. Jo dared to ask the question: are we simply shifting the bottleneck?
Each of these distinguished experts also spoke about their experiences of person-centred care, how it has impacted their practice and how Therapeutic Radiographers can start to think about adopting its lessons.
Recapping the first day, Spencer Goodman, chair of ARC and professional officer for radiotherapy at the SoR, said: “It went really well. Person-centred care was the core, but we can’t do that without the workforce. Today achieved that.
“We covered the big picture, and the breakout sessions brought together the national pieces. Deep, professional, but warm and welcoming, with lots of excellent presentations.”
The evening closed with a delicious three-course gala dinner, an onsite DJ and a dance party that lasted late into the night.


Day 2 – light at the end of the tunnel
ARC resumed the following day with radiographers returning to the conference hall for a conversation with a professional patient, Elizabeth Smith. Elizabeth is a Therapeutic Radiographer and a professional swimmer who was diagnosed with Hodgkin Lymphoma in 2022. “There wasn’t a fear of the unknown,” she explained. “I did find some comfort in that I was getting treated where I worked!”
The compressed timeline in which Lizzie was diagnosed, began treatment and concluded it, she said, changed her perspective on the patient experience. “You spend the whole treatment period looking for the light at the end of this tunnel, and then, when it comes, it’s such a feeling of joy,” Lizzie said.
“It’s so easy as a Therapeutic Radiographer to get carried away with the race to get the next patient in. But they are all individuals. It’s all about grounding yourself, asking how they are and listening to the answer they give. We also need to learn where we can direct these patients to get the appropriate help.
“Talk to the partner too. The patient has been prepped to the nth degree, but the person sat next to them has found themselves in a world they weren’t expecting. There should be a bit of consideration for that person. You will always remember how they interacted with you, and how they made you feel.”
Lizzie’s talk was followed by a Q&A session, as attendees sought her perspective on how they could help make that patient experience more comforting, supportive and empowering.
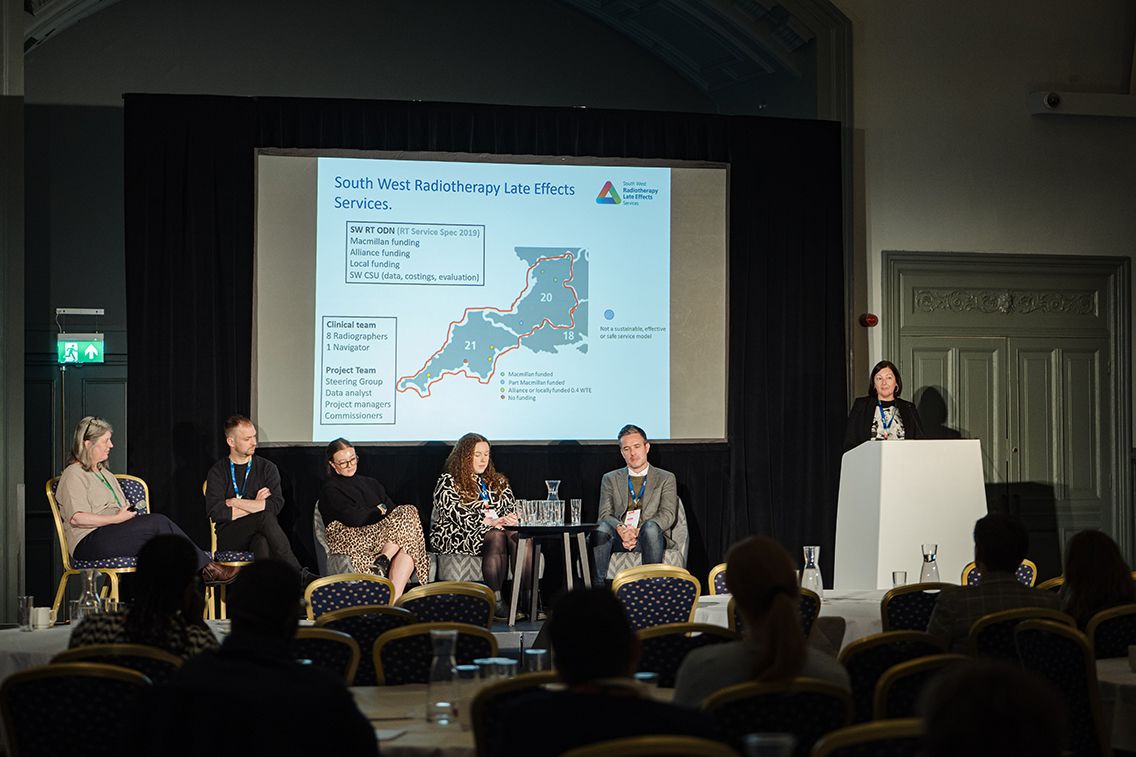
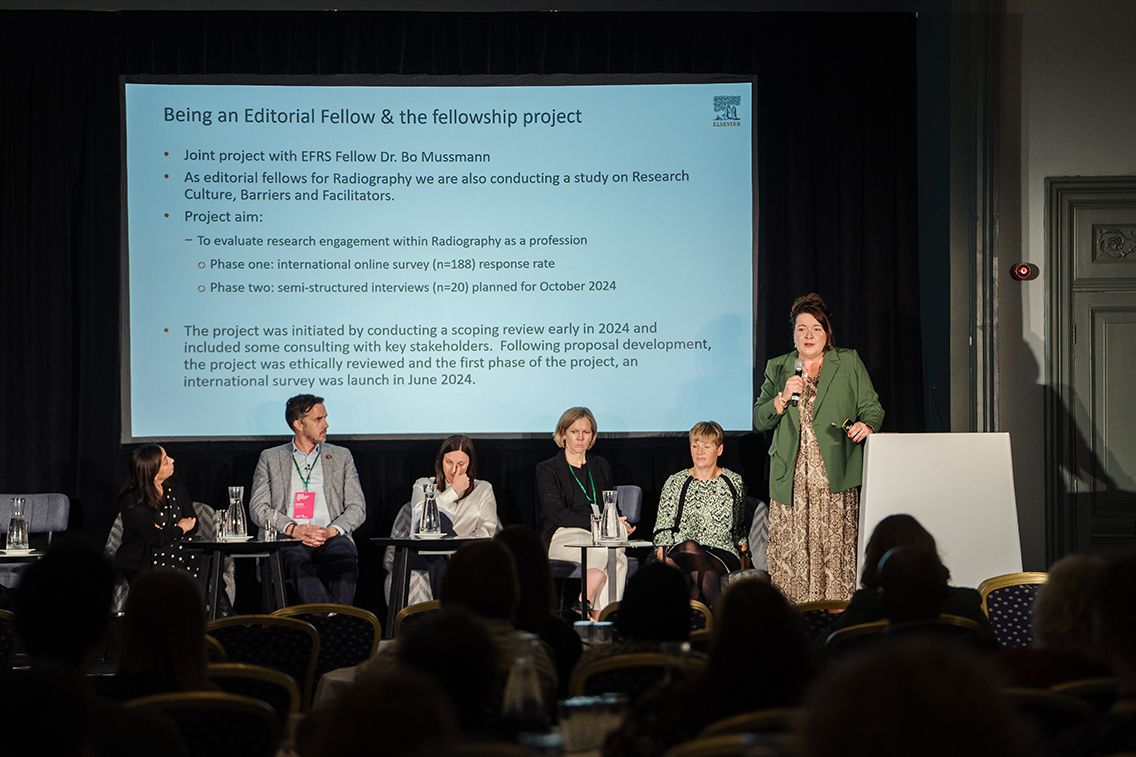
Following a break to return to the exhibition hall, the audience returned to more breakout sessions for proffered papers.
On the second day, these sessions included:
Rachel Harris | The Patient/Carer Voice: How loud is it?
- The patient/carer voice can be a powerful driver of service improvement and lead to interventions that are tailored to their needs and preferences.
Melanie Clarkson | Empowering Individuals through Workforce Development
- Workforce development is crucial for the success and growth of any organisation. Policy documents to assess an increase in the support workforce along with enhanced, advanced and consultant levels of practice.
Suzanne Jordan | Caring For Our Professionals: Wellbeing Underpinning Service Delivery
- The number of patients being referred for radiotherapy continues to increase, meaning that the benefits of hypofractionation schedules on demand are temporary. It could be argued that creating more time for Therapeutic Radiographers to deliver personalised care is key to not only retention but the psychosocial wellbeing of staff. How do we achieve that?
“This conference has covered the entire breadth of radiotherapy, from technology to person-centred care,” said SoR professional officer Dr Laura Charlesworth. “There’s so much to take from this – the conference has been sorely missed. It’s great to be back with this unique community.
“The highlight has been seeing all these connections happen in front of my eyes. Everyone is sharing their experiences and their knowledge, and going back to their departments with connections that will drive their practice forward.”

Gallery

Read more
More about the Annual Radiotherapy Conference
The Annual Radiotherapy Conference is a two-day event organised by the SoR, where interactive panels and contemporary proffered paper sessions provide an enriching and immersive environment for learning, meeting peers and sharing best practice.
Image credit: Eva Slusarek