The growth and progression
of PET-CT
PET-CT has grown dramatically in the UK over the past 20 years but what challenges lie ahead?
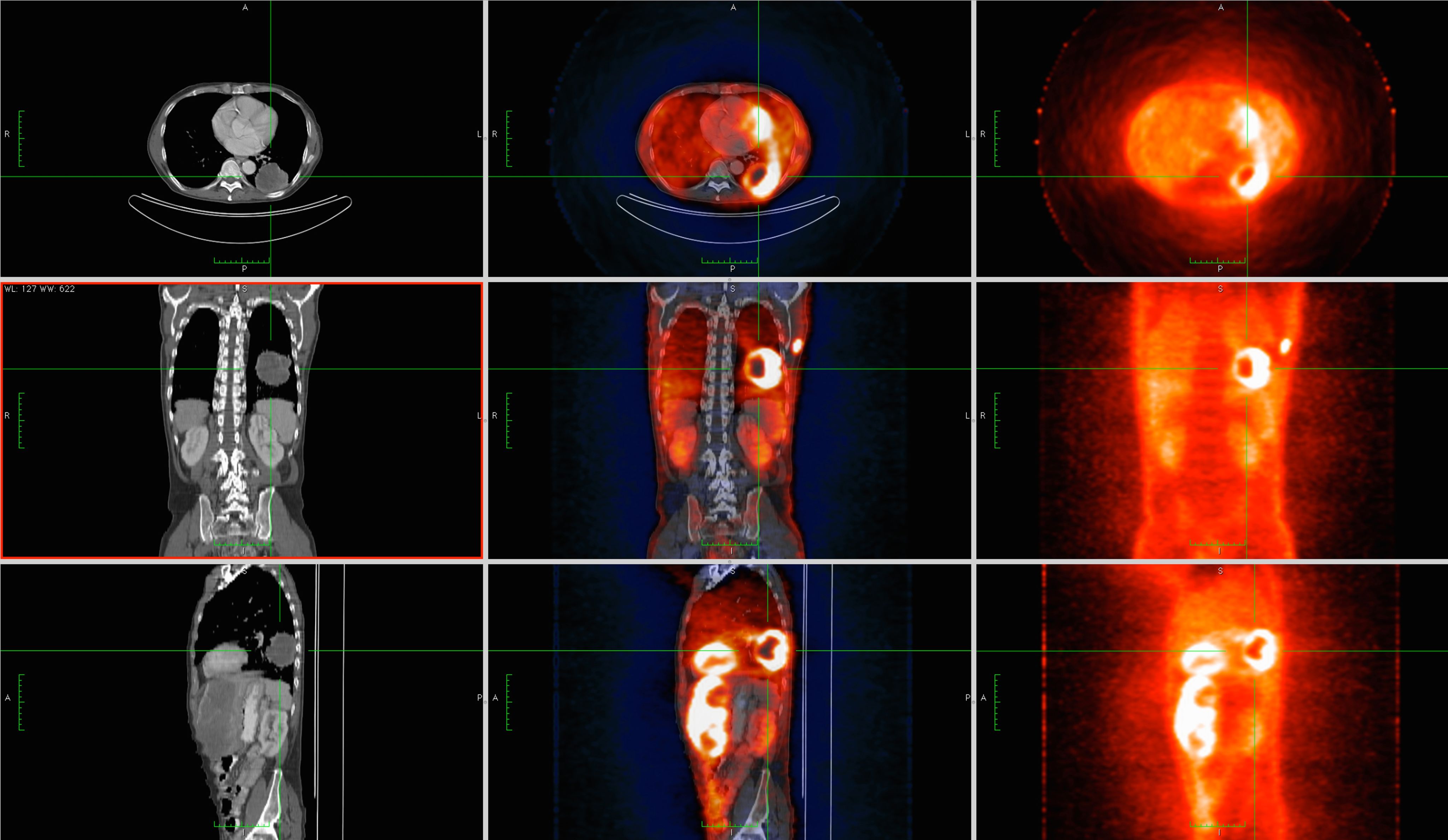
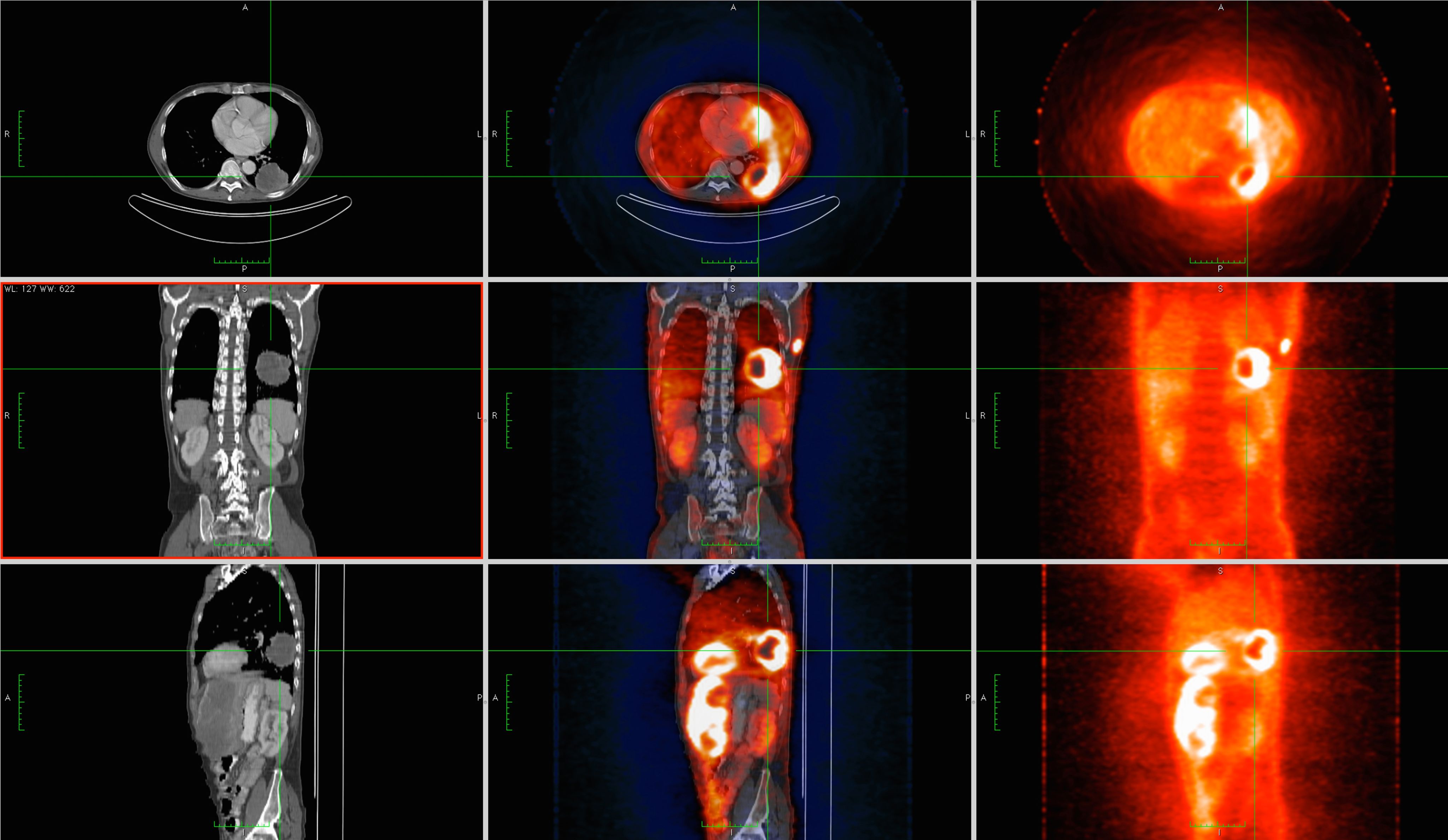
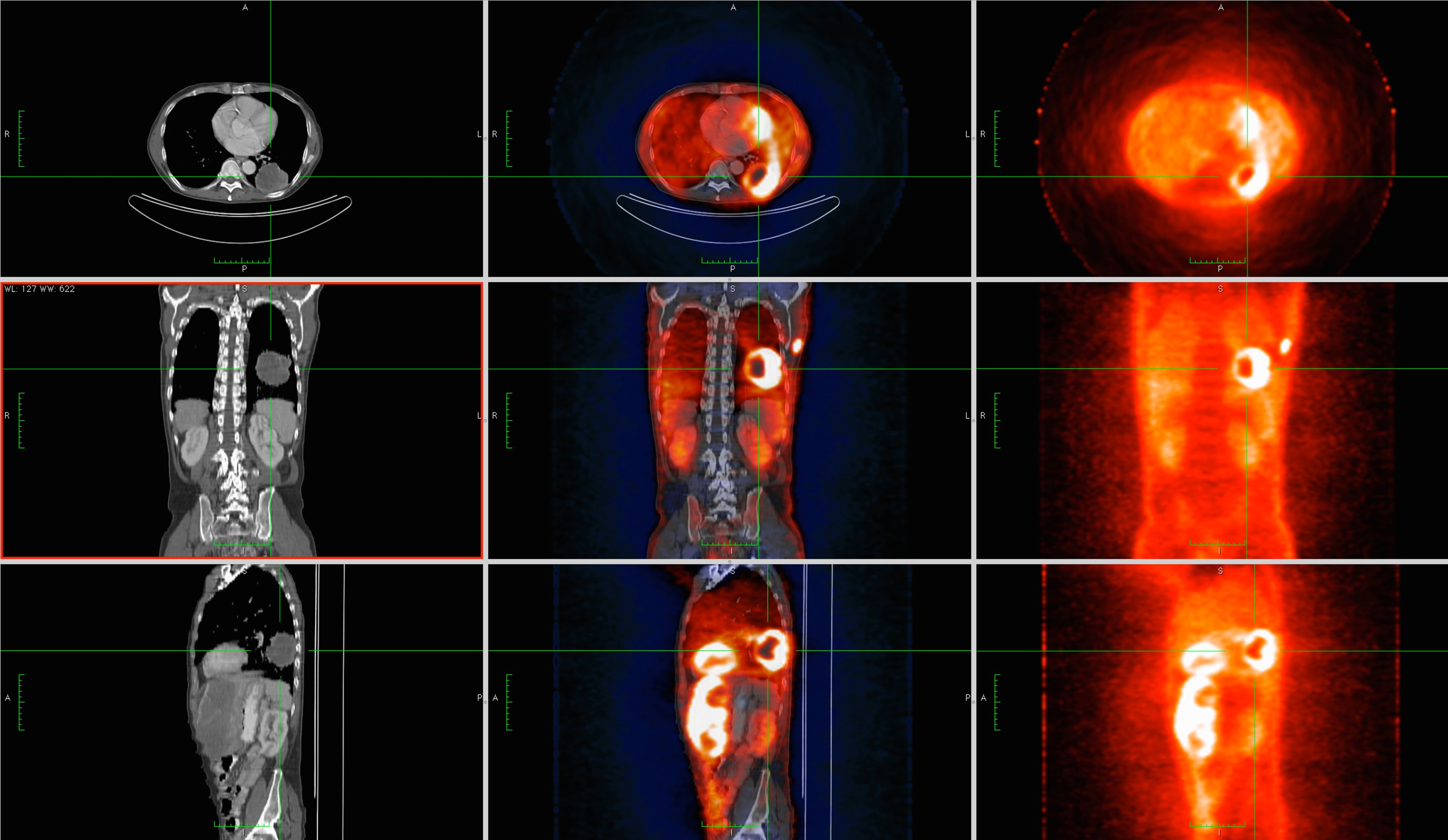
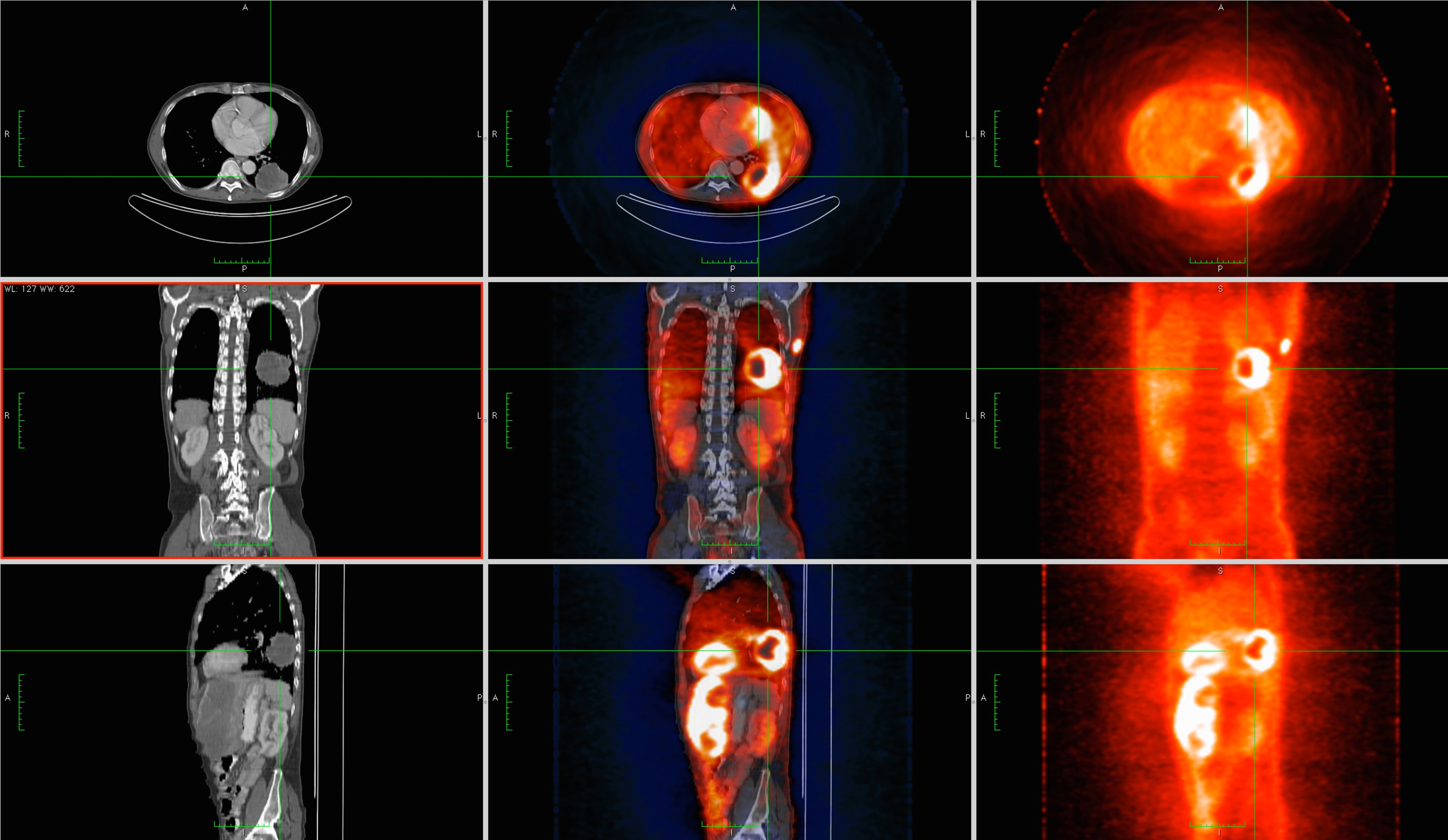
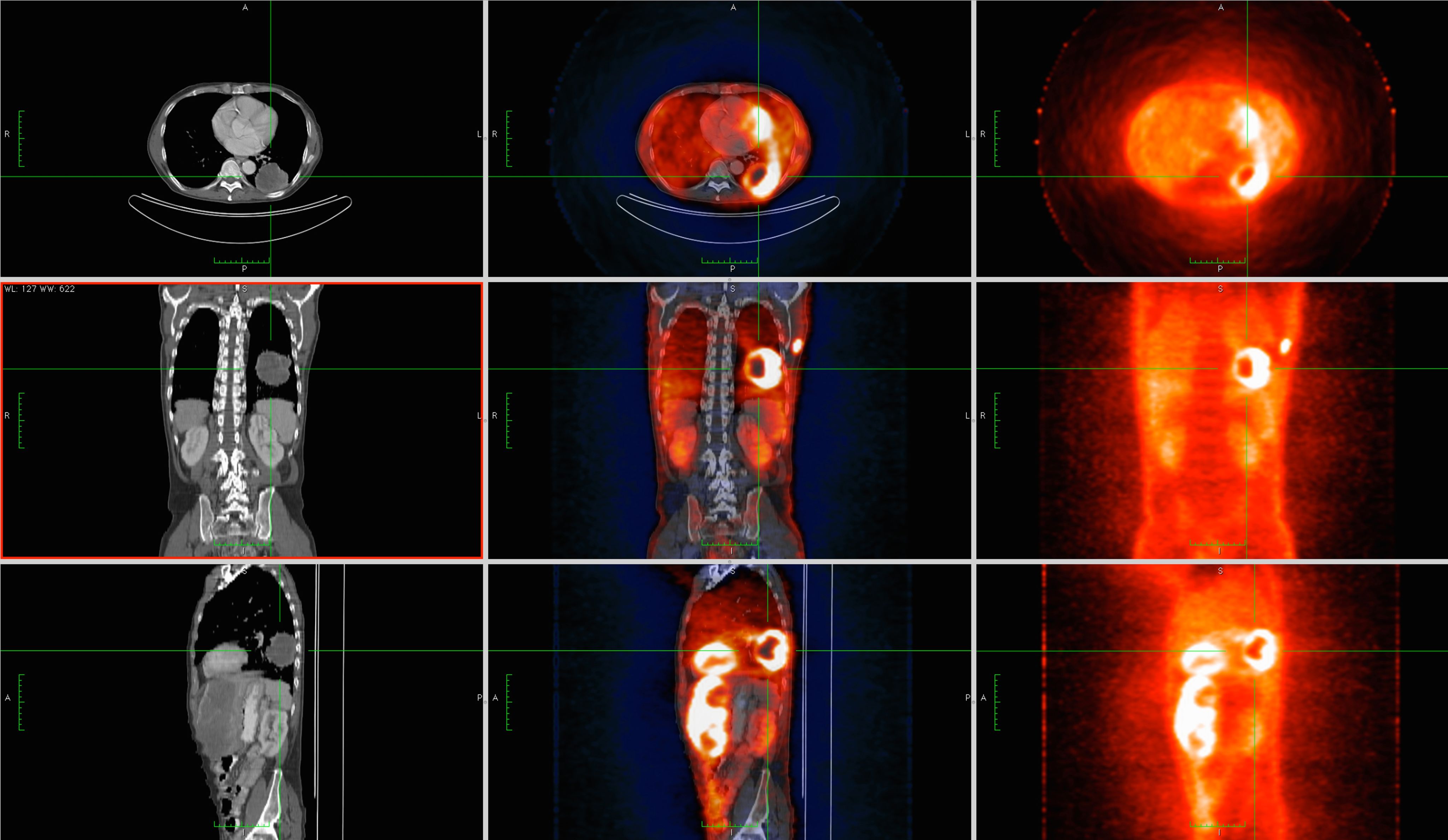
Positron Emission Tomography (PET) is a functional imaging technique that allows non-invasive, in vivo imaging. This article provides an overview of provision progression over the past two decades and provides a review of the current role of PET-CT imaging in the UK, posing current challenges and opportunities.
The beginning of the 21st century saw the continuing development of PET imaging technology across the US and Europe. However, the turning point, from a technological perspective, was the introduction and use of X-ray CT to compliment PET as a means of attenuation correction and anatomical localisation. Today we mainly refer to PET as PET-CT. Almost all systems in use clinically across the UK are PET-CT systems. By 2003, PET-CT technology had been successfully established, however, as with many innovations, cost and raising awareness of the value of an innovation can be an overwhelming factor in preventing a new concept being realised.
Michael Bedford and Michael Maisey, like many other professionals exposed to PET, were very aware of the value of PET in oncology and the importance of provision availability. They set out to review the requirements for a PET cancer imaging service. The UK was used as an example to create an algorithm for calculating the infrastructure requirements to support the demand for PET studies in lung cancer, later extended to all oncological indications in the UK and Europe. The findings highlighted the requirement of considerable investment in this technique. In 2003, there were just seven PET scanners in the UK with a suggested 49 additional scanners required to fulfil the demand of all oncological examinations. The UK had the least sufficient infrastructure at 14%, in comparison with other European countries, such as Belgium, which had the most sufficient infrastructure, operating with 197% sufficiency1. The requirement to develop PET and accessibility was ever more evident.
In 2005, the Department of Health (DH) released the paper ‘A framework for the development of PET Services in England’. The framework was developed by the DH at the request of strategic health authorities and specialised commissioning groups. Its intention was to guide commissioners and potential providers of services by delivering advice in areas such as the benefits of PET scanning, available technology, number of scanners required, training and workforce issues2. The framework was sent out for public consultation in July 2004 and, in response, a working party was established by The Royal College of Radiologists (RCR) in collaboration with the Royal College of Physicians, the Intercollegiate Standing Committee on Nuclear Medicine, the British Nuclear Medicine Society (BNMS) and Institute of Physics and Engineering in Medicine. The working party sought to make the framework a reality through the release of the report PET-CT in the UK. A Strategy for Development and Integration of a Leading-Edge Technology within Routine Clinical Practice3.
These documents proved to be key in the drive of PET provision and service development. Approximately 11,000 scans were being performed per year in 2005 and almost 40,000 in 2009. Professor Sir Mike Richards, national clinical director for cancer and end-of-life care, wrote to specialist service directors detailing the success of the PET-CT UK strategy, bringing the UK into a much stronger position with access to PET-CT services at a rate of 800 scans per million population. By 2012, England was up to 1,257 scans per million population. While progressing well, England still lagged behind Italy with 5,144 scans per million population. Unfortunately, accurate data reflective of Europe is difficult to source reliably beyond 20144.
As previously highlighted, by 2012 investment and collaboration in the form of the multidisciplinary working party resulted in a remarkable increase in service provision, providing 51 scanners (42 static and nine mobile) covering a total of 54 locations, almost doubling scanner access from 2007 to 2012. Approximately 71,000 scans were performed in 2012 and the growth of PET continued to rise at a rapid rate5.
Growth over the past decade
Over the past decade, we have observed a growth of more than 300% in PET imaging. The Richards report also predicted the PET-CT volume growth, and NHS statistics for 2020/21 are reflective of that growth prediction (Figure 1).
Figure 1. Count of NHS imaging activity 2012/13-2020/21 (England)5
The value of PET to alter and influence treatment pathways in oncology is pivotal to this growth. One of the key influencers in ensuring provision is accessed appropriately is the evidenced-based review of referral guidelines.
Referral guidelines
Evidence-based guidance is essential when supporting decisions to select patients for PET imaging. It is important that a PET-CT referral clearly details the clinical question to be answered and considers how the scan may alter patient management.
In 2005, there was a limited group of referral indications, which had been selected based on research and best practice at that time. The guidance was again reviewed in 2009 and in 2013, opening the referral criteria indications as increasing evidence supported the value of PET imaging. Figure 1 presents the year-on-year growth for the past 10 years, and it can be demonstrated that following the referral guidelines update there was a significant increase in PET-CT growth of up to 36%, averaging approximately 14% growth year on year until Covid-19 hit in 2020. In 2020, PET referral volumes remained static with just 0.3% growth, reflective of PET-CT oncology service concerns around the height of the Covid-19 pandemic5. Figures 2a and 2b provide a graphical representation of the PET-CT referral criteria case mix in 2012 compared with today in 2022: (tap or hover over data points to show numbers).
Figure 2a. PET-CT referral criteria case mix in 2012
Figure 2b. PET-CT referral criteria case mix in 2022
Increased scanning provision and the revised referral guidance updates for PET-CT have had a positive influence on the growth and awareness of PET in the past 10 years. According to the National Cancer Research Institute (NCRI), the latest figures reflect that there are currently in the region of 80 PET-CT services, mainly at fixed site locations, delivering circa 200,000 scans per year, reflective of the 2020-2021 data6. This growth has continued to surpass predicted levels, which have typically sat at 12% growth. While this is a very significant and positive outcome for the patient population, as this marks improved access to services, this comes with a logistical challenge for service delivery – first, due to workforce challenges and, second, due to radiotracer availability.
PET-CT workforce – challenges and opportunities
Nuclear medicine (NM) and PET-CT are specialist imaging modalities with an extensive multidisciplinary workforce, which makes strategic planning difficult due to the vast range of professionals involved. These include radiographers, technologists, clinical scientists, radiologists, NM physicians plus many more.
Focusing on the imaging practitioner (radiographer/technologist), nationally we continue to face the same challenges recognised 10 years ago7. There are limited undergraduate training schemes for NM, which complicates recruitment for this already hard-to-recruit specialty, coupled with the registration challenge for the undergraduate technologist programme. Many organisations bridge this gap by employing radiographers and training them in NM. While this provides the cross-pollination important to hybrid imaging environments, it sometimes leads to loss of depth and breadth within the specialty.
At the time of writing, a new undergraduate course for the NM technologist has been launched for 2022, the first of its kind in the past three years, again taking the opportunity to bridge the workforce gap within the NM profession. This by no means resolves the challenges we face if courses cannot remain viable due to low recruitment numbers, or if the professional registration parity between the radiographer and technologist is not addressed. The lack of professional regulation and registration to own this workforce makes recruitment to a standard even more challenging. The BNMS launched a registration campaign in 2020 with the aim of addressing this issue8.
Universities running diagnostic radiography programmes also recognise the significant workforce challenge the profession faces, with some universities taking the opportunity to restructure their training programmes to provide opportunities for undergraduate radiographers to experience NM and PET-CT in their final year, allowing the student to move into a specialism with base experience and theory as a qualified graduate.
While employers and universities persevere with existing challenges, we must, as a profession, look to a solution. Our suggestion would be to introduce a clear and structured workforce plan and training framework!
While training and recruitment are a key part of workforce planning, retention and succession planning are also critical factors. Leaders and managers have a responsibility to navigate their way through service challenges to ensure funding for staff development and retention to sustain vital services. More and more organisations are reliant on in-house mechanisms for succession planning, taking the opportunity to maintain service resilience with a "grow-your-own" approach. Furthermore, Covid-19 regulations have exacerbated service gaps for onboarding new staff and retention has been compounded further by Brexit, resulting in a loss of staff.
The complexities of managing large teams calls for good leadership and clarification of roles. Multicultural teams present a wealth of diversity and uniqueness, which could pose challenging due to natural variation in culture and understanding. Organisational culture and leadership play a crucial role in embedding corporate values, ensuring policies protect against discrimination, support equality in the workplace and demonstrate ethical professional values that focus on key objectives, while celebrating differences to enhance performance. In the absence of a framework, this is hard to achieve. Multicultural teams fostered in a nurtured environment offer the unique ability of competitive advantage and operational efficiencies through faster shared learning from diverse experiences and expertise to achieve better staff retention9.
Radiotracer availability
The other significant factor in the growth of PET and stability of established services is cyclotron access and tracer production reliability. Various radioactive isotopes can be produced in a cyclotron. For PET, the isotopes must be capable of positron emission and have a desirably short half-life.
Commercial isotope (tracer) production in PET is focused on Fluorine-18 18F, with a half-life of 110 min. The tracer most prevalently used is 18F-Fluorodeoxyglucose (FDG), which is used for approximately 85% of PET imaging cases and is focused on oncology cases.
Alternative 18F tracers in use are:
- 18F – NAF for bone imaging.
- 18F – PSMA for prostate imaging.
- 18F – brain imaging agents Amyloid and Tau.
- 68Ga – prostate and neuroendocrine tumours.
Research/academic facilities are typically using Flourine-18, in addition to the following:
- Carbon-11 C11 with a half-life of 20 minutes.
- Nitrogen-13 N13 with a half-life of 10 minutes.
- Oxygen-15 O15 with a half-life of 2 minutes.
Commercial production of 18F-FDG has become well established across the UK for several reasons.
- Increased demand and the requirement for oncological studies, which remain the mainstay (90%) of the workload throughout clinical centres in the UK.
- The cost of 18F-FDG has reduced.
- There is a support network for commercial cyclotron facilities and locations are strategically placed. In the event of 18F-FDG production failure, backup production in most cases is sourced from another cyclotron facility. Figure 3 presents the current cyclotron locations in the UK and Ireland.
Figure 3. Current cyclotron locations in the UK and Ireland
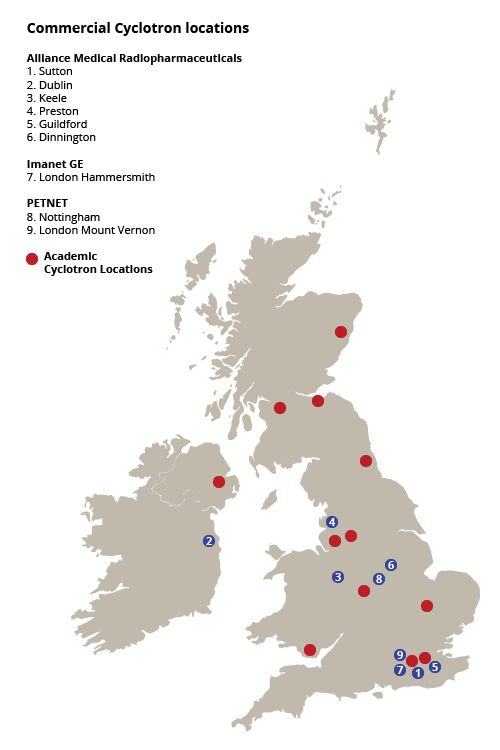
Nonetheless, while 18F-FDG production and availability has significantly improved over the past decade, over recent years there has been a growth and demand challenge combined with a technology replacement/refurbishment requirement. Cyclotrons require upgrading and this process is ongoing. With one cyclotron out of action for upgrade, the same tracer requirements are still necessary but are shared among neighbouring cyclotrons, placing additional volume demand on the supporting cyclotron site. Furthermore, there is a requirement to develop the market for non-FDG tracers that may have widespread clinical use. PSMA, as an example, is the tracer of choice for prostate imaging and, at the time of writing, demand is high, the forecast being spring 2022 when access to 18F-PSMA should alleviate as the latest cyclotron upgrade is completed. Furthermore, there are many more non-FDG tracers with robust evidence of the clinical benefit, deliberated in several papers delivered by the NCRI PET Research Network (PRN)10.
Research
The NCRI funded a PET research initiative to support and encourage all aspects of PET research in the UK, from the role of PET in clinical care to the development of clinical trials and radiotracer development. Subsequently, the PET Research Steering Committee and the PRN have been established with the aim of providing an interface with scientific and medical communities and the NHS10.
As previously discussed, one significant drawback that PET currently faces is the limited availability of non-FDG tracers and this was one of the conclusions highlighted by the PRN. New tracers are understandably more expensive than FDG but costs are currently significantly higher, which, in the current economic climate, makes purchase difficult to justify. In addition, there is limited availability and new tracers are not available in all parts of the UK. This, in turn, compounds the cost as transport costs are equally high. A suggestion by the PRN to help with this problem would be to consider commercial/academic partnerships for novel tracers. This is certainly an avenue that requires consideration11.
What is clear from the PRN research is that, regardless of development in PET provision, there remains a significant number of issues that need addressing to assist PET research development in the UK – particularly for non-FDG tracers – as this will assist in the development of PET beyond the FDG oncology workload. One suggestion was to create a comprehensive online database, cataloguing UK PET trials and pre-clinical activity. This resource can be accessed by the PET community and is now live on the PRN website. This is a valuable tool to see current trials available, in progress and centre activity. The NCRI PRN is certainly a resource that PET users should utilise10.
PET imaging – the future landscape
When considering the future landscape for PET, it would be remiss not to touch on PET-MRI and acknowledge its UK presence. Currently there are five research MRI scanners in the UK and work continues at the research facilities in developing this modality, with a focus in many centres on neurology. Further reading is recommended on PET-MRI, particularly a recent competencies and training review published in 2020, highlighting similar training challenges to PET-CT due to the complex workforce structure 11.
Another area of focus when we consider the future landscape of PET and nuclear medicine is the future of PET with theranostics. Theranostics is the new wave of bespoke personalised treatment reducing radiation burden to the patient. It can often be complex, for example, accompanied by an interventional theatre procedure, as in the case of radioembolization with Sir-Spheres or multiple imaging time points for dosimetry (131-MIBG imaging for targeting NETs). These procedures are on the incline, calling for close partnerships and cross-service collaboration to ensure optimal planning and utilisation of operational resource and capacity. Ra-223 and Lu-PSMA, for example, can be delivered on an outpatient basis over several fractions, thus negating the need for hospitalisation and detracting from bed occupancy resources on the wards. These radiotherapeutics are not always commissioned or have tight restrictions for eligibility, often through links with trials, preventing free access to all. It is essential, therefore, that further focus and work is required as proof of concept to encourage commissioners to make these services available to all service users on a more equitable basis.
Summary
Over the past two decades, we have seen PET develop into an imaging modality that has changed the face of oncology imaging worldwide.
This article has highlighted how the UK has faced challenges, like many countries, in the development of PET provision and how these have been overcome. Most significantly, the collaboration of the key disciplines in PET to develop a working party and a strategy for PET-CT to enable the UK to meet targets of a 1,000 per million scan population and go beyond this to bring the UK in line more closely with neighbouring European countries. Nonetheless, 10 years on, there remain areas that require further development as a matter of urgency. The most significant is workforce review and the requirement of a structured workforce plan, which considers training and regulatory parity for the radiographer and technologist.
Furthermore, in the advent of technological advances, it is essential to recognise that commercial organisations, clinical and academic, also have a role to play in the development of PET provision. Efforts must be cooperative and coordinated if they are to be successful. The provision of radiotracer availability, development, research and training must be closely linked to infrastructure, both in terms of specialised facilities in which to train staff, and in delivering adequate numbers of trained personnel to meet future skill and capacity requirements.
Angela Meadows is Head of PET CT Clinical Services at Alliance Medical and Adviser to the Society of Radiographers Nuclear Medicine and Molecular Imaging Advisory Group.
Rayjanah Allie is General Manager, Nuclear Medicine at University College London Hospitals.

References
1. Bedford M and Maisey M. Requirements for clinical PET: comparisons within Europe. Eur J Nucl Med Mol Imaging. 2004. Feb;31(2): 208-21.
2. Department of Health. A Framework for the Development of Positron Emission Tomography (PET) Services in England. Oct 2005 (gateway reference 5265).
3. The Royal College of Radiologists. PET-CT in the UK. A Strategy for Development and Integration of a Leading-Edge Technology Within Routine Clinical Practice. 2005.
4. Richards M and Denton E. Predicted Demand for PET-CT Services in England. Department of Health (Gateway Reference 13215) 2010. Available at http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_110859.pdf
5. NHS. Diagnostic Imaging Dataset. 2021. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/diagnostic-imaging-dataset/diagnostic-imaging-dataset-2020-21-data/
6. UK PET facilities. Available at www.ncri-pet.org.uk/researchers_scanning_facilities.php
7. Wareing A, Meadows A and Leadbetter H. A Review of Radiographic PET-CT Education Provision in the UK – Current Status 2011. Robert Gordon University, Aberdeen, Alliance Medical Ltd, Preston, UK.
8. British Nuclear Medicine Society. Statutory Registration for Nuclear Medicine Technologists. Available at www.bnms.org.uk/page/StatutoryRegistrationforNuclearMedicineTechnologists
9. Hajro A, Gibson CB and Markus P. Knowledge exchange processes in multicultural teams: linking organizational diversity climates to teams’ effectiveness. 2014. Academy of Management Journal, 2014, 60 (1), 345-372.
10. Gilbert F, Fleming I, Marsden P et al. How to Increase Availability of Non-Fluorodeoxyglucose Radiotracers for PET Research in the UK.
11. Mada MO, Hindmarch P, Stirling J et al. Competencies and training of radiographers and technologists for PET/MR imaging – a study from the UK MR-PET network. European J Hybrid Imaging 2020 4, 1 (2020). Available at https://doi.org/10.1186/s41824-019-0070-6

